A staggering statistic reveals that over half a billion people globally lack adequate healthcare due to geographical or financial constraints. The emergence of telemedicine is changing healthcare delivery and offers remote consultations with qualified professionals. This technology-driven approach breaks down geographical limitations, opening doors to a world where quality healthcare is accessible from the comfort of your home. So no wonder that the telemedicine market is expected to soar to USD 330.26 billion by 2029, from USD 172.44 billion in 2024.
Now, the traditional doctor’s visit, often fraught with long wait times and inconvenient scheduling, is undergoing a significant transformation. We don’t need to imagine a scenario where a simple video call allows us to discuss a rash with a dermatologist or receive guidance on managing your diabetes. This is a reality we can experience within a few clicks.
In this article we’ll explore the various forms this technology takes, the undeniable benefits it offers patients and providers alike, and the exciting advancements shaping the future of telemedicine.
Telemedicine vs Telehealth
Services that allow for interactive, two-way communication between providers and consumers, patients, or caregivers, all without the need for physical proximity are commonly described as telehealth and telemedicine. Although these are distinct terms, they are often used interchangeably, which often causes confusion. World Health Organization defines the two concepts as the following:
Telemedicine means receiving medical care from a doctor or healthcare provider remotely. It focuses specifically on using technology to deliver clinical services and medical consultations virtually. This includes doctor-patient consultations, remote diagnosis, and treatment conducted through telecommunications technology.
Telehealth extends beyond clinical care to include activities like remote vital sign monitoring, patient education, and administrative meetings. It broadens the scope of healthcare delivery beyond traditional clinical settings to encompass various health-related services accessible from a distance.
| Area | Telemedicine | Telehealth |
| Scope of Services | Virtual medical care and services | Clinical and non-clinical activities |
| Applications | Focuses on remote clinical care, consultations, and diagnosis. | Includes various healthcare services, such as remote monitoring, education, administrative meetings, and more. |
| Technological tools | Focuses on video conferencing, remote diagnostic tools, and EHRs for clinical consultations. | Includes a broader range of technology such as wearables, apps, and communication systems. |
| Examples | Virtual doctor-patient consultations, remote diagnosis. | Health education resources, mental health support, chronic disease management, administrative meetings. |
Despite these differences, the terms overlap significantly when it comes to delivering remote healthcare. This overlap is why they are frequently considered synonymous in casual use, though in professional contexts, the distinctions are more carefully observed.
Types of Telemedicine
Direct-to-consumer Telemedicine (Synchronous Telemedicine)
DTC telemedicine allows patients to contact healthcare providers directly from their homes or other locations through telecommunications technology. A study found that the global market size of DTC telehealth services is expected to reach USD 520.85 million by 2031, from USD 292.9 million in 2021.
This model is closest to a traditional in-person consultation and appeals particularly to patients who seek immediate care without the wait times associated with in-person visits. A study conducted by Kaiser Permanente examined 1,274 patients who had video calls over a three-month period and found that patients generally were satisfied with the experience. 93% of the surveyed patients reported that the video visit adequately addressed their needs, and 84% noted that having a video visit improved their relationship with their provider.
We may consider Teladoc, Amwell, Lemonaid, and Doctor on Demand to be the most popular DTC telemedicine apps among others.
Store-and-Forward Telemedicine (Asynchronous Telemedicine)
Store-and-forward (SAF) telemedicine involves healthcare providers sharing patient data with a specialist at a different location. This method does not require the presence of both parties simultaneously and employs a wide range of mediums, such as photos and forms, in addition to video and voice.
Common applications include dermatology, radiology, and pathology, where images, biosignals, or other medical data are collected, stored, and then sent to a specialist for review. The Center for Connected Health Policy noted that asynchronous telehealth facilitates more efficient peer consultations among primary care providers and specialists.
In fact, the majority of Americans express satisfaction with asynchronous telehealth services. A survey conducted in February 2022, with 1,301 US adults, revealed that 69% supported legislative efforts aimed at expanding access to asynchronous telehealth. Additionally, 82 % of healthcare workers also voiced support for the expansion of asynchronous telehealth services.
Some of the most popular SAF telemedicine apps are DermEngine, MoleScope, SnapEGC and Visibly among others.
Core Telemedicine Statistics
In September 2019, the World Health Organization forecasted a potential healthcare crisis by 2030, with up to 5 billion people lacking access to healthcare. The COVID-19 pandemic intensified global healthcare concerns, bringing them to the forefront. Unfortunately, billions still lack adequate healthcare access, and over half a billion have fallen into extreme poverty due to healthcare expenses. Here is where telemedicine emerges as a pivotal solution that revolutionizes healthcare delivery by expanding access to quality services and potentially reducing costs. Let’s have a look at the key statistics that prove that telemedicine is here to stay.
Patient Adoption Statistics
- 83% of patients who engaged in a telemedicine visit in the previous year expressed their intention to either maintain or boost their utilization of telemedicine in the future.
- Approximately 60% of patients who had a telemedicine visit in the previous year engaged in at least three virtual consultations. Among them, over one in five participated in six or more visits, with similar frequency observed among patients with and without chronic illnesses. Additionally, nearly 76% of patients who had a telemedicine visit reported improved access to healthcare services.
- Around 34% of patients who had a virtual care visit within the previous year utilized telemedicine to discuss medications or refill prescriptions, while approximately 20% used it to review test or treatment options. Remarkably, patients with chronic illnesses showed particularly high usage of telemedicine for these services.
- 85% of patients claim that their overall care was either better or similar with virtual care, and more than half reported increased satisfaction.
- 70% of all surveyed patients expressed a likelihood of consulting a doctor for non-emergency situations if the visit could be conducted virtually.
Source: Doximity
Doctor Adoption Statistics
- More than 83% of physicians acknowledge the utility of telemedicine in enhancing continuity of care for patients with complex or chronic conditions. Nearly 65% mentioned that telemedicine improved communication with their patients.
- Almost 84% of physicians reported using telemedicine on a weekly basis, with 40% integrating it into their daily clinical practice. Psychiatrists had the highest daily usage at 84%, followed by endocrinologists at 57%.
- Routine follow-up visits stand out as one of the most predominant applications in 92%. Additionally, 57% of physicians utilize telemedicine for discussions regarding lab and test results, as well as treatment options with their patients, with oncologists showing an even higher usage rate in 70%.
- 66% of surveyed physicians noted at least one time management benefit, including enhanced autonomy and work-life balance, increased productivity, and simplified schedule management.
- About 61% of surveyed physicians noted a decrease in their patient no-show rates since implementing telemedicine, likely attributed to the enhanced convenience, accessibility, and flexibility of virtual visits. 77% of physicians observed either equivalent or improved patient adherence to treatment plans through telemedicine.
- 88% of physicians said that telemedicine has increased patient access to health care. Approximately 44% of physicians discovered that telemedicine has decreased wait times for their patients, whereas 41% mentioned that telemedicine has broadened their community reach and referral networks. (source: Doximity)
All in all, the evolution of telemedicine from its inception to the present day signifies a significant transformation in healthcare delivery. Integrating the latest telemedicine trends into your medical facility is essential for improving remote patient care.
Trends in Telemedicine
Generally, we never know what the next boom will bring us. No one could ever have predicted COVID pandemic and the boost it gave to telemedicine industry growth. Chances are we could still sit and strategize over the infinite possibilities of health tech growth. However, many things remain, and as they become more common, we may predict what directions of care delivery may benefit the most. For example, a huge big trend is the use of advanced technologies like 5G networks, artificial intelligence (AI), and internet of things (IoT) devices in healthcare. So let’s review the trends that in a couple of years will be our new norm.
Adoption In Virtual Primary Care and Hybrid Care Models
Amwell´s study has shown that over half of all consumers anticipate using telehealth more frequently post-COVID-19 compared to before the pandemic, while 92% of providers plan to continue offering video visits even when in-person appointments are safe. Both physicians and consumers are open to using telehealth for various purposes such as chronic care check-ups and post-surgery follow-ups. Additionally, for many types of consultations, patients express a preference for virtual appointments with their doctors.
Technology Integrations
Healthcare services are increasingly integrating with cutting-edge technologies, including high tech software and devices. A significant player is 5G. Its faster network speed will allow efficient delivery of medical images, remote patient monitoring, virtual meetings, and more. Real-time technology enabled by 5G can also play a vital role in determining equipment, medications, and other healthcare needs of the telemedicine industry.
Employer-based Care
A study found that 94% of employers prioritize managing healthcare benefit costs as their top concern over the next few years to address the increasing healthcare prices due to rising inflation or provider consolidation. More employers are incorporating telemedicine into their healthcare benefits and offers employees medical consultations as a standard part of employment benefits. Additionally, 95% of employers anticipate further enhancing affordability efforts by incorporating virtual medical and behavioral healthcare. Other positive data reveal, 55% believe that virtual care and telehealth will contribute to lowering healthcare costs over the next three to five years.
Growing Trend Of Asynchronous Telemedicine Care
Asynchronous telemedicine is becoming more prevalent, since it allows patients and healthcare providers flexibility by communicating and sharing information on their own schedules. Jon Salon, the president of MDLive, pointed out that asynchronous care offers healthcare providers an efficient method to prioritize and manage common conditions, reducing up to 90% of administrative workload. This approach allows providers to allocate more time to patients who really need it and offer a cost-effective option for urgent and basic healthcare needs. A rise in adoption is anticipated among younger consumers, who prefer asynchronous interactions for managing various aspects of their lives over live conversations.
Adoption of AI
AI is being implemented more broadly in telemedicine that results in automated interactions with patients. When integrated with medical information e.g. symptoms, medications, treatments, doctors, and conditions, healthcare chatbots offer a time-saving solution. In fact, AI applications can increase the speed and accuracy of the diagnosis process. The FDA approved the first AI-based diagnostic device that detects potential signs of diabetic retinopathy. After uploading high-quality photos, the algorithm accurately identified the disorder in 87% of cases and correctly identified individuals without the disease 90% of the time.
Online Patient Reviews
Consumer feedback is becoming crucial for healthcare providers’ growth and reputation. A recent study found that 74% of consumers consider online patient reviews crucial when making healthcare decisions. These reviews can either encourage or deter patients from choosing a particular doctor or clinic. Moreover, another survey found that 80% of consumers trust online reviews as much as personal recommendations.
Increased Digital accessibility
As per a KeyCare survey, convenience is a priority for many consumers and 45% prefer telemedicine for minor urgent issues over in-office visits. While retail health brands are prioritizing online appointments, healthcare organizations improve the visibility of telemedicine services and invest in online appointment booking processes to meet consumer preferences. In fact, a Kyruus study found that 40% of consumers prefer online appointment booking and approximately half of this group is open to switching to another provider to have this option available.
Challenges in Telemedicine
As transformative as telemedicine is, it brings with it a set of challenges that healthcare providers and patients must navigate. From technical issues such as poor internet connectivity and system design flaws to broader concerns like patient privacy and the handling of controlled substances, these challenges impact the efficiency of telemedicine in healthcare.
Lack of Access to Needed Technology
Access to necessary technology remains a significant barrier for some patients. Not owning or understanding how to use devices like smartphones or computers limits their ability to benefit from telemedicine. Elderly individuals, minorities, and those with lower socioeconomic status may face barriers accessing the technology required for virtual visits. In fact, a recent report showed that regarding providers’ perceptions of the types of patients finding video visits most challenging, 86% cited older patients, while 37% pointed to patients lacking technology skills or access to the internet/system.
Poor Internet Connectivity
Inadequate internet connectivity adversely affects telemedicine sessions. Poor audio and visual quality makes it difficult for doctors to communicate effectively and accurately diagnose conditions. Jordan Hill, an assistant research scientist with Indiana University´s School of Public Health, mentions: “If you’re doing video conferencing, you would need an internet connection – preferably a high-speed internet connection – which, again, depending on how rural you are, that may be a factor that limits your ability to make use of telemedicine. You also, you need some kind of technology that will allow for that video conferencing.”
Provider´s Technical Problems
Technical issues on the provider’s end, such as software glitches or hardware failures, can interrupt telemedicine services. 80% of providers noted insufficient technical support, while nearly two-thirds reported encountering technical issues frequently. It can lead to delays and reduces patient confidence and satisfaction in digital healthcare.
Inefficient or Challenging System Design
Telemedicine platforms that are not user-friendly can discourage use, particularly if they are complicated or unintuitive. A study showed that 49% of technical challenges were due to a challenging system design, which made patients and doctors unable to log in or connect audio. This can hinder widespread adoption among healthcare providers and patients.
Fraud & Abuse
Telemedicine’s digital interface opens possibilities for false billing and unauthorized access to patient data. This can pose significant legal and ethical challenges. Healthcare providers can safeguard patient information by enforcing cybersecurity protocols, encrypting communications, conducting frequent security assessments, and providing training to staff on privacy and data protection protocols.
Controlled Substances
The remote prescription of controlled substances via telemedicine requires careful regulatory compliance to prevent misuse and addiction. The Journal of Community Empowerment for Health pointed out that some controlled substances require a valid prescription obtained through at least one face-to-face consultation before they can be prescribed, distributed, and delivered. Lack of compliance can cause inefficiency in prescriptions management and monitoring.
Patient Privacy
Patient privacy in telemedicine is not negotiable. The risk of data breaches and unauthorized access threatens to expose sensitive personal health information when not addressed accurately. More and more video conferencing platforms are exploring the development of more secure options for telemedicine appointments. Additionally, Hill suggests overcoming data security concerns by opting for telemedicine appointments and sharing information over the phone.
Telemedicine may appear to have both positive and negative aspects. While it provides cost savings, convenience, and broader access to care, it also faces challenges such as the mentioned above. A survey by The Associated Press-NORC Center for Public Affairs Research shows that the majority of adults aged 18 and older are open to using telemedicine services for various reasons. According to the survey, 88% of adults are comfortable with the idea of using telemedicine for medical consultations, ongoing chronic illness management, or urgent health concerns, either for themselves or for older loved ones they care for.
Benefits of Telemedicine for Patients
A Jefferson Health study assessed 650 patients over eight months and found that telemedicine is not only cost-effective but also capable of addressing the majority of patients’ health issues. Among the 650 patients, 74% had their healthcare concerns resolved during their telemedicine consultations. Promising numbers, right? Let’s dive into these and other advantages of telemedicine for patients.
Remote Second Opinion
Telemedicine offers patients the convenience of obtaining a second opinion from specialists remotely. It ensures better-informed decisions without the need to travel. In fact, 85% of patients claim that their overall care was just as good as virtual care, and more than half reported increased satisfaction.
Telemedicine in Rural Areas
In rural areas, telemedicine significantly reduces barriers to healthcare access, providing residents with services that might otherwise be unavailable locally. For example, studies showed that teleophthalmology frequently enhances healthcare access, thereby facilitating patient screening and diagnosis.
Ease of Communication
Telemedicine simplifies communication between patients and healthcare providers, facilitating more frequent and direct interactions through digital platforms. Informing patients about health issues encourages them to monitor their progress and interact more with their physicians, ultimately enhancing their cardiovascular risk. A systematic review undertaken by Polisena et al. revealed that home telemonitoring improved clinical outcomes for congestive heart failure (CHF) patients compared to traditional treatments.
Catch Problems Early
Regular telemedicine check-ins enable early detection of health issues, improving outcomes through timely intervention and management. A study showed that incorporating ophthalmology examinations into smartphone applications offers a convenient means to measure visual acuity, helping in the diagnosis and treatment of various eye conditions like glaucoma or amblyopia. This approach ensures patients receive timely and appropriate treatment and referrals to specialists when necessary.
Better And Easier Access To Specialists
Telemedicine eliminates geographical barriers, allowing patients easy access to a broader range of specialists, enhancing care quality and options. For instance, smaller medical practices may not have specialists on-site. However, telehealth provides the opportunity to connect with specialists from other healthcare facilities. Additionally, patients have the opportunity to collaborate with specialists from across the globe.
No Need To Take Time Off From Work
Telemedicine consultations can often be scheduled during convenient times, reducing or eliminating the need for patients to take time off from work. A respondent from a study claimed: “Another good aspect of it, I think, is I can be home, and I don’t have to drive anywhere and take extra time away from work. So, all I have to do is simply switch to a portal, stay logged in for work, take my 30 minutes. My 30 minutes is done, I can go right back to working. I don’t have to take that travel time. I don’t have to be out of the office”
Benefits of Telemedicine for Doctors
Telemedicine technology reduces operational costs and minimises patient no-shows. It also expands patient reach, streamlines workflows, and provide physicians with tools that improve patients outcomes. Let’s take a closer look on the benefits of telemedicine technology for doctors.
Virtual Therapists Are More Sustainable
Operating virtually, therapists can reduce overhead costs such as office space and travel. A study revealed a significant reduction in the time patients spent accessing healthcare, with a decrease of 56% observed when using telemedicine compared to conventional health services. Additionally, they found that the average maintenance cost was slashed by an impressive 94% making their practice more environmentally and economically sustainable.
Fewer No-Shows
With the flexibility to schedule appointments according to their own daily routines, patients are less prone to last-minute cancellations or no-shows. According to a survey, about 61% of physicians noted a decrease in their patient no-show rates since implementing telemedicine, likely attributed to the enhanced convenience, accessibility, and flexibility of virtual visits.
Possibility to Serve More Patients
It allows doctors to serve more patients across wider geographic areas, potentially increasing their patient base and income. A study conducted on dermatologists and their patients proved that teledermatology consultations were shorter than face-to-face appointments. Dermatologists also agreed that it simplified the process, which made them serve more patients.
Increased Capacity
By enabling more efficient scheduling and management of patient care, telemedicine enhances healthcare providers’ capacity. An examination of the implementation of telemedicine in Malaysia proved that hospitals and other facilities could provide timely advice to critical patients without waiting for a specific specialist. This led to optimized resource utilization, reduced mortality and morbidity rates, and minimized patient transfers. Overall, organizations were able to achieve significant cost and resource savings compared to traditional approaches.
Reduces Doctor’s Workloads
It automates or streamlines basic tasks such as prescription refills and patient monitoring, reducing the workload on doctors. Around 34% of patients who had a virtual care visit within the previous year utilized telemedicine to discuss medications or refill prescriptions, while approximately 20% used it to review test or treatment options.
Direct Patient Control
It gives doctors more direct control over their schedules and patient interactions, allowing for more flexible and efficient practice management. It’s not a surprise that patients often struggle to recall post-surgical instructions. Through apps, doctors can offer reminders to patients in the comfort of their homes. This approach enhances patient adherence to instructions, leading to improved clinical outcomes. Additionally, telemedicine enables healthcare providers to stay well-informed about the patient’s current condition and monitor any symptoms remotely.
Seamless Patient Record Collection And Consolidation
Telemedicine facilitates the efficient collection, storage, and consolidation of patient records, improving data accessibility and management for healthcare providers. According to a recent study, doctors typically review scheduling requests and patient profiles, enabling them to manage the patient queue and filter patient profiles effectively. Cloud-based medical record-keeping ensures data protection for telemedicine data, including patient information and recorded video consultations.
In short, without a doubt, telemedicine is beneficial for both patients and healthcare providers. Through telehealth, neither the provider nor the patient needs to spend time traveling, saving valuable time. Patients gain access to necessary healthcare services at reduced costs. Meanwhile, for providers, telehealth enables the efficient management of multiple patient appointments per day, potentially leading to increased revenue streams.
Telemedicine Examples
Telemedicine’s versatility and widespread application across various medical specialities illustrate its transformative impact on healthcare delivery. In this section, we will explore concrete examples of telemedicine in action through a review of top telemedicine apps and specific use cases in different medical fields. From remote cardiac monitoring systems to digital solutions for mental health and specialized services like dermatology and orthopedics, these examples highlight how telemedicine technology is used to enhance patient care and streamline provider workflows.
TOP 6 Telemedicine Apps
Halodoc
Halodoc is a healthcare app that allows users to consult with doctors via video, voice, or chat. It encompasses specializations like midwife care, diabetes management, heart health, vaccinations, mental wellness, pet care, and parenting support. It provides health support services such as stress assessments, body mass index tracking, pregnancy calendars, anxiety and depression screenings, and donation facilitation. Moreover, it offers features like drug delivery and lab test bookings, enhancing accessibility and convenience for patients.
Maple
Maple is a Canadian telemedicine platform that connects patients with doctors for on-demand consultations using text or video. Their primary objective is to minimize waiting times and offer top-notch healthcare services 24/7. The app provides immediate medical advice, prescriptions, and referrals, focusing on accessibility and quick healthcare delivery. Additionally, it provides convenient doorstep delivery of medications and offers family healthcare plans.
doxy.me
Doxy.me is a free telemedicine solution used globally by healthcare professionals. It offers video calls without requiring patients to register or download the software. It is easy to use and accessible, with a strong emphasis on maintaining patient privacy and security. With its user-friendly interface and comprehensive features, Doxy.me emerges as one of the leading telemedicine apps for providers, streamlining healthcare delivery.
Teladoc
Teladoc is one of the largest telemedicine services in the U.S., providing 24/7 access to healthcare professionals via phone or video for non-emergency medical concerns. Users can consult with doctors via the app for common conditions like colds, flu, and allergies, receiving a diagnosis and treatment plan. The app also includes a symptom checker to aid users in understanding their condition and navigating the consultation process with a doctor.
Amwell
With over 1.5 million downloads, it provides users with access to a provider’s overall rating and experience, allowing them to select doctors based on their backgrounds and expertise. It offers general urgent care services for common ailments like colds, flu, strep throat, sinus infections, and cold sores. Additionally, Amwell provides speciality services such as therapy, psychiatry, pediatrics, breastfeeding support, nutrition counselling, and women’s health.
Lemonaid
Lemonaid is a telemedicine application focusing on virtual consultations for minor illnesses and prescription services. Users can seek medical advice from doctors for a range of conditions, including common ailments like UTIs and colds, and receive a diagnosis along with a treatment plan. Additionally, the app includes a symptom checker and medication reminder function. Lemonaid also allows users to conveniently refill existing prescriptions directly through the app.
Telemedicine Use Cases
The practical applications of telemedicine span across various healthcare areas, offering access to medical services and improving patient care. From primary care to specialized fields such as dermatology, optometry, cardiology among many others, telemedicine is overcoming geographical barriers, and enhancing patient outcomes. Let’s dive into some key examples.
Telemedicine in Primary Care
Primary care providers, including physicians, nurse practitioners, and physician assistants use telemedicine to assess, diagnose, treat, and manage a wide range of common health concerns through virtual consultations, video conferencing, and other digital platforms. It also enhances continuity of care, facilitates collaboration with specialists and other healthcare professionals, and helps patients better manage their health conditions.
Apps like Teladoc and Amwell facilitate primary care via telemedicine, broadening access to basic health services.
Telemedicine for Dermatologists
Through video calls or photo uploads, dermatologists can examine a patient’s condition and provide a diagnosis and treatment plan in high-definition video and audio, ensuring HIPAA-compliant privacy. Dermatologists consult for skin conditions such as acne, eczema or psoriasis, evaluate skin lesions, prescribe medications, monitor treatment progress among other services.
Dermatologists use apps like DermEngine and First Derm to provide remote consultations, allowing for the evaluation and management of skin conditions through uploaded images and videos.
Telemedicine for Nurse Practitioners
NPs assess, diagnose, treat, and monitor patients’ health conditions through virtual consultations, video conferencing, and other digital platforms. They consult for common acute conditions such as colds and flu, manage chronic conditions such as diabetes, monitor treatment progress and much more.
Nurse practitioners engage in telenursing through platforms like Doxy.me and SimplePractice, offering remote patient monitoring, health education, and follow-up care.
Teleneurology
Telemedicine technology in neurology enables neurologists to diagnose, treat, and monitor patients with neurological conditions through virtual consultations, video conferencing, and remote monitoring tools. Telehealth neurologists can conduct comprehensive evaluations, assess symptoms, review medical history, and order diagnostic tests remotely. They can also provide education, counseling, and treatment recommendations. Telemedicine neurology offers early detection of neurological disorders, and ongoing management of chronic conditions such as epilepsy, stroke, and Parkinson’s disease.
Apps such as Teleneurology.com and NeuroCall provide specialized virtual neurology, helping diagnose and manage conditions on time.
Teleoptometry
It allows optometrists to provide eye care services, such as vision testing, eye examinations, and prescription of glasses or contact lenses, without the need for an in-person visit. Optometrists can remotely assess visual acuity, screen for eye conditions, and discuss treatment options with patients, providing personalized care. It also allows for timely interventions, early detection of eye problems, and ongoing management of vision-related issues.
Apps like EyecareLive and SimpleContacts offer remote vision tests and consultations about eye health.
Orthopedic Telemedicine
Through telemedicine, orthopedic specialists can assess patients’ orthopedic concerns, provide medical advice, and develop treatment plans without the need for face-to-face visits.
Orthopedic telemedicine includes video consultations, remote monitoring of rehabilitation exercises, and the transmission of medical images such as X-rays and MRI scans for interpretation. It allows timely interventions, early detection of orthopedic issues, and ongoing management of musculoskeletal conditions, such as arthritis, sports injuries, and fractures.
OrthoLive and SimplePractice are examples of apps facilitating virtual orthopedic consultations.
Telemedicine in Cardiology
Cardiology telehealth allows to diagnose cardiovascular conditions, and manage treatment plans without the need for in-person visits. It encompasses various video consultations, remote monitoring of cardiac devices, and the transmission of medical data like electrocardiograms (ECGs) and echocardiograms for interpretation. Cardiology telemedicine also enables timely interventions, early detection of cardiovascular issues, and better management of chronic conditions like hypertension and heart failure.
Telehealth cardiology apps like CardioSecur and Heartbeat Health provide platforms for cardiologists to monitor heart health remotely.
How Empeek Can Help
Drawing on our expertise in healthcare technology and software development, Empeek assists in the development of telemedicine apps across various specialties. We understand the criticality of adhering to US standards and legal regulations concerning the collection and storage of PHI. With our extensive experience collaborating with US healthcare providers, coupled with a dedicated team of professionals, we offer everything necessary to revolutionize your approach to treating patients remotely. See for yourself how Empeek excelled in telemedicine solutions tailored to our clients´ requirements and main objectives.
Remote Cardiac Monitoring System
The Remote Cardiac Monitoring System we developed for our US-based client provides a sophisticated solution for 24/7 cardiac health monitoring. This system sends real-time cardiac data to specialists who identify abnormalities. The results are quickly forwarded to doctors for review, enabling informed medical decisions based on daily data fluctuations observed by both patients and doctors.
Patients use a compact, mobile ECG device from home that includes a patient diary feature for noting daily activities. An intelligent algorithm automatically filters and categorizes data, emphasizing high-risk abnormalities and alerting technicians to urgent cases. Our expert team developed a system that allows for customization, tailoring data collection to specific groups like athletes or children with differing heart rates, ensuring accuracy and relevance in monitoring.
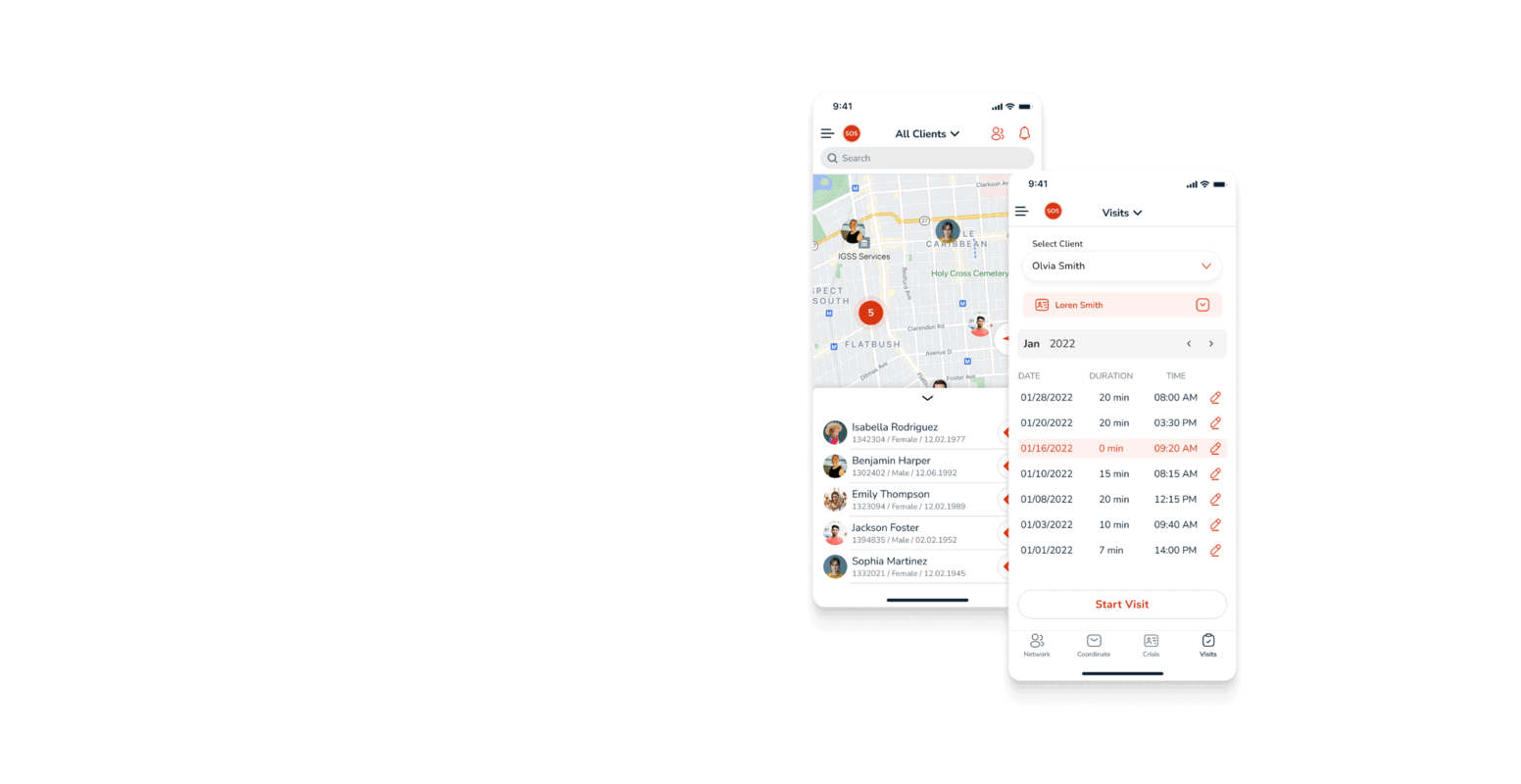
Digital Mental Health Solution
We developed a Digital Mental Health Solution for the US-based company VelloHealth. The goal of the project was to enhance the operational efficiency and clinical effectiveness of Assertive Community Treatment (ACT) teams. Its primary telehealth objectives are to ensure the safety of ACT team members, comply with financial and clinical best practices, and integrate seamlessly with Electronic Medical Records (EMR) through a one-way interface.
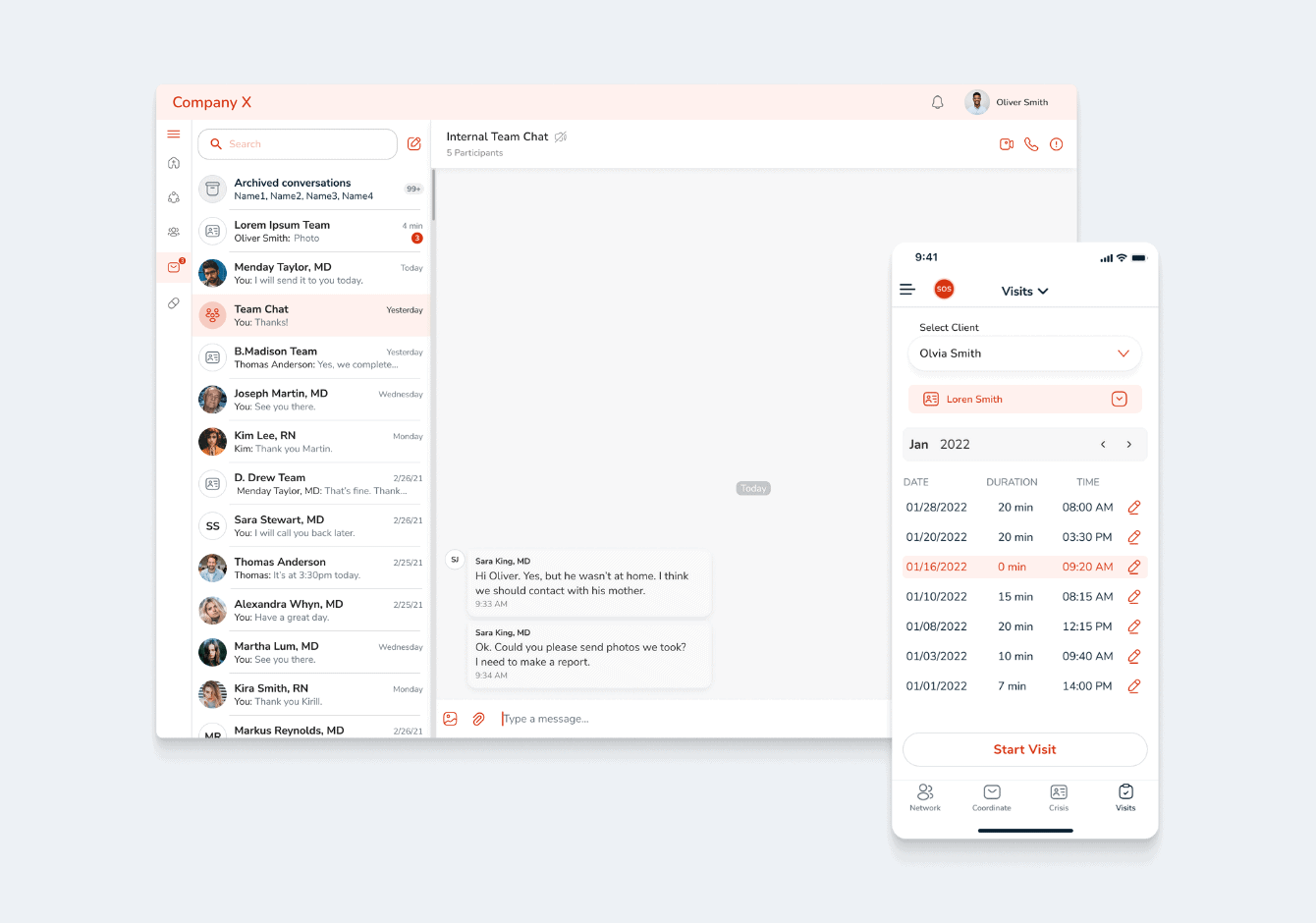
ACT team members use this platform to collaborate extensively on patient assessments, treatment planning, and daily interventions. Unlike traditional models where practitioners manage individual caseloads, this approach fosters collective responsibility among team members to ensure each client receives comprehensive services necessary for recovery from mental health issues.
Empeek designs solutions are designed to improve safety, compliance, and efficiency, integrating into your current medical practices. Learn more about how Empeek’s telemedicine apps development services can transform your healthcare delivery. Contact us today and discover how they can benefit your organization and patients.
Bottom Line
Telemedicine isn’t here to replace the irreplaceable value of a face-to-face doctor’s visit. It’s here to be a game changer, a powerful tool that expands access, empowers patients, and streamlines healthcare delivery. As a patient, we can expect continued advancements in convenience, with AI potentially offering preliminary consultations and real-time data analysis for even more streamlined diagnoses. We also become even more active participants in our health journey, while doctors can build stronger relationships through frequent virtual interactions.
As technology like 5G networks becomes more widespread, the potential for even more sophisticated virtual consultations becomes a reality. We are on our way of creating a healthcare landscape that is accessible, affordable, and empowers individuals to prioritize their well-being like never before.