Around 6.2 million Americans suffer from heart failure (HF), a chronic condition that prevents the heart from pumping enough oxygen into the body. This impaired cardiac function leads to other diseases and malfunctions, decreases life expectancy, and worsens the quality of life. Luckily, due to the global implementation of telehealth, and ever-improving medical device technologies, medical providers can effectively supervise the HF-related biological parameters and adjust treatment.
Telemedicine and telemonitoring already showed its positive impact in heart failure management through improvements in physical quality of life in patients, self-care maintenance and efficient time usage. However, several challenges have surfaced, such as implementation cost, regulatory constraints, and data privacy, that need to be carefully addressed.
Let’s review the importance of telemonitoring, its challenges and adoption in heart failure management, and how Empeek can make remote patient monitoring a norm in your practice.
Challenges in Monitoring Patients with Heart Failure
Finding an effective treatment for congestive or chronic heart failure means improving the quality of life and increasing the life expectancy of more than 6.2 million people in the USA alone. Monitoring certain biological parameters is the basic step to do it. To show you that it’s an urgent matter, as well as a market opportunity, we’ve gathered recent statistics from the American Heart Association reports, heart failure clinics, and ongoing HF research.
- Heart failure is the leading cause of hospitalization worldwide
- 13.4% of deaths in the USA are caused by HF
- 64.34 million cases – current global prevalence of HF
- 20-25% of hospital readmissions within 30 days are patients with HF, and almost 50% of patients are hospitalized within the year after initial admission
- 346.17 billion USD – global expenditure for managing and treating patients with HF
- 915,000 new cases of HF are diagnosed annually
The statistic shows the urgent need for developing consistent and effective HF treatment management. Where to start? With measuring and controlling the clinical variables such as heart pressure, heart rhythm, oxygen saturation level, implantable cardiac device performance, etc. And here both patients and doctors face a few challenges.
- Lack of awareness regarding the HF risk factors. Most people with high HF risk don’t know they are in a risk group or live a lifestyle that increases their chance of HF development.
- Lack of accessibility. Not all patients have timely access to medical aid due to their location, social status, insurance coverage, etc.
- Poor education regarding how to properly measure the needed parameters.
- High cost of in-patient monitoring implementation
The good news is that there is a way to respond to these challenges by adopting telemonitoring technologies. These include sensors, mobile applications, software that connect the patients with the doctors and system, invasive monitoring of implantable telemonitoring devices, and so on. While telemedicine for patients with heart failure has just started to become a global norm, it has already shown its efficacy. So what are the benefits of remote cardiac monitoring in the care of patients with heart failure?
Benefits of Telemonitoring in the Care of Patients with Heart Failure
With so many factors that influence the HF patient’s condition, it’s natural to ask the most important question: what can be telemonitored in heart failure patients? Below is the list:
- Bodyweight
- Heart rate
- Blood pressure
- Body temperature
- Oxygen saturation level
- Heart rhythm
- Central venous and pulmonary arterial pressure (invasive telemonitoring via implantable devices)
The tricky part is that the results of telemonitoring have value when they are structured, analyzed, and powered with algorithms capable of recognizing the negative pattern. This is the reason for implementing the holistic telemonitoring infrastructure that connects the patient’s data, patient, providers, and medical care personnel to ensure access to data, its interpretation, and quick response. In our previous article, we explored how IT companies transform cardiac care with remote monitoring now, let’s discover the effects of telemonitoring on patients with heart failure.
Decrease of Hospital Readmission Rate
Analyzing the result from the sensors and apps can alarm about the negative changes in the organism before it causes life-threatening conditions. A systematic review by Cochrane, covering 41 studies on telephone support monitoring for HF patients, revealed a 34% decrease in all-cause mortality and a 20% reduction in HF-related hospitalizations. These findings align with another meta-analysis by Anker et al. A study tracking over 200 HF patients with reduced ejection fraction for 18 months found a low rate of decompensation-related admissions without an increase in mortality.
Predicting the Emerging Acute Cardiac Decompensation
Another thing where telemonitoring in patients with heart failure serves well is detecting the acute cardiac decompensation risks. Monitoring the patients’ weight over a certain time helps in evaluating the decompensation occurrence risk and planning proper medical intervention. Solutions as Cardiogram, Biobeat, and Biotricity among others help to prevent decompensation episodes and enable timely medical interventions
Providing Specialists with Real-Time Data
This is especially useful for patients with implanted cardiac devices (ICDs). Being able to track their activity and performance will allow the doctor to better assess the patient’s condition and prescribe the proper treatment or plan the change of the device that is monitored. Startups, as OneProject, Spire, and Cardiomatics among others, are the game changers in providing physicians with actionable real time data. It can be used to adjust prescriptions, modify diagnoses, or provide more streamlined and effective care.
Increasing the Patient’s Role in Treatment
Despite heart diseases being the leading causes of death in the USA, many people, including those diagnosed with HF, have poor knowledge of HF symptoms, treatment, and measures that can prevent one from developing it. Being involved in the telemonitoring process either by regular interviewing by a specialist nurse, controlling the measurements from the sensors and providing them to your doctor, or changing one’s habits to ensure a better quality of life increases awareness of the patient of his role in improving the outcomes.
Managing the Patients Flow & Plan Interventions
This is among the top benefits of telemonitoring in heart failure management, especially for larger clinics and hospitals. Observing changes in the patient’s medical conditions allows clinics to identify the risk group, plan intervention, prepare for patient’s hospitalization and emergency care, manage doctors’ workload, etc.
The value of telemonitoring and telemedicine in heart failure management is obvious as when used consistently, it will improve the patient’s outcome and treatment quality. It comes, however, with challenges you need to know before adopting it. Read about them below to have a strategy in advance.
Improvements in Self-care Maintenance
Telemonitoring improves patient self-management capabilities and empowers individuals to take a more active role in their healthcare journey. Research indicates that patients expressed a sense of control over their well-being and a closer connection to their medical team. In fact, patients who incorporated telemonitoring into their self-monitoring routine achieved faster blood pressure control compared to those who relied solely on self-monitoring. Findings from the INTERACT study revealed a significant 16% enhancement in adherence when text messages were used during follow-up. This suggests that such interventions play a crucial role in reducing the occurrence of heart failure and other related events over the long term.
Better Physical Quality of Life
Studies show that telemedicine can significantly alleviate depressive symptoms and enhance the quality of life for individuals managing heart failure, especially those experiencing moderate depression. Additionally, telemedicine reinforces the patient’s role in heart failure self-management and promotes patient empowerment. It serves as a powerful tool for continuous education, self-care promotion, and therapy adherence. Patients often report feeling more in control of their disease and experiencing a closer connection to their medical team, that leads to heightened feelings of safety.
Time Utilization
Telemedicine has brought significant changes to the way doctors manage their time during clinic hours. While consultations are perceived to be shorter, it offers the convenience of working from home and potentially reducing travel time. Additionally, patients save time, effort, and expense of traveling to the hospital. They appreciate the environmental benefits of avoiding unnecessary travel. Waiting for video consultations at home is preferred over hospital waiting rooms.
Challenges of Implementing Telemonitoring and Telemedicine in Heart Failure Management
The implementation challenges usually revolve around its costs, change of cooperation dynamic between patients and doctors, data privacy, equipment, and software quality. Let’s review them in more detail.
Implementation Costs
Expenses associated with infrastructure include equipment acquisition, maintenance, depreciation, and subscription to telemedicine platforms. However, every case is unique and so is its budget. Adopting telehealth reduces healthcare costs, but they depend on the type of product, development time, the technology used, integrating it with the existing system or setting up from scratch, etc. Taking into account the benefits it has, it might be a solid investment into your business to make it more market-competitive. Understanding HIPAA compliance is also an important factor during the development of the telehealth system.
Change of Patient-Doctor Approach
A study revealed that both patients and providers focus on four key aspects of their relationships:
- establishing rapport and building alliances,
- the level of provider attentiveness during video visits,
- gaining insights into patients’ lives and living conditions,
- navigating communication challenges.
With the implementation of telemedicine, each of the above aspects were altered and required adaptation from both patients and providers. It requires patients to familiarize themselves with the new procedures and engage with providers in the new way. Also, an integration of telemonitoring platforms with healthcare CRM software can give you a hand in improving the patient experience and data flow management.
Data Privacy
As sensors and various ICD collect the patient’s health information, its management should follow all the state and federal law requirements. The failure to do so may cause plenty of legal troubles, which is why you always should talk about it with your developers. We have an article that will give you a basic understanding of data handling in medical IoT.
Reimbursement Policy
Studies prove that one of the primary hurdles for implementing, expanding, and widely adopting telemedicine in HF is the reimbursement policies set by national regulatory agencies. These reimbursement policies lead to disparities in telemonitoring accessibility across different countries. In fact, in 2018, state telehealth policies varied in adoption. Nearly all states (98%) reimbursed for interactive communication, 57% for Store and Forward, and 45% for Remote Patient Monitoring. Most states implemented parity policies: 73% for commercial payers, 63% for Medicaid, and 86% for location.
Regulatory Constraints
National regulatory limitations, especially those concerning data protection, security, and privacy, serve as significant hurdles. The rapid pace of technological advancements frequently outstrips the ability of regulatory bodies to keep pace, resulting in outdated guidelines and legal ambiguities. In fact, currently, providers must navigate federal policies, potentially 50 different state policies, and numerous private plan policies. This complexity has significantly deterred the use of telemedicine.
Technological Constraints
Some of the most prominent technical challenges in telemonitoring are infrastructure constraints, interoperability, and health information management. This includes limited access to stable internet connectivity, which creates barriers to the effective implementation of telemedicine. Additionally, poor connectivity leads to difficulties in data transmission to result in delays and errors when exchanging crucial healthcare data. This impedes diagnosis and treatment planning processes.
Adherence by Patient and Caregivers
Telemonitoring involves active participation of patients and caregivers, which create challenges in its effectiveness. Non-invasive telemonitoring involves patients engaging in daily self-evaluation routines, which are then transmitted to a care facility. If signs of hemodynamic decompensation are detected, this prompts a therapeutic response. However, to ensure patients or caregivers adhere to this routine long-term pose challenges. To address this, telemonitoring providers turn to wearables (such as smartwatches and sensors embedded in clothing), automatic data collection and analysis. It also relies on algorithms for detecting hemodynamic decompensation and initiating therapeutic responses. In fact, future advancements will likely incorporate the Internet of Things for continuous and seamless monitoring of health status.
Telemonitoring is constantly broadening its range of services, from supporting various use cases to introducing new digital devices. With the main goal to improve the patient care process and treatment results. Yes, handling these challenges can be burdensome if you don’t have a team that can create a telemonitoring system without compromising your provider’s reputation and company’s credibility. Empeek has enough experience and knowledge base to get the project done. One of the relevant examples is a real-time health monitoring system we have developed recently.
The Future of Telemedicine in the Management of Heart Failure Patients
Immersed Wearable Technology and Remote Monitoring
An essential factor driving remote patient monitoring programs forward is the evolution of wearable technologies. Both medical devices are becoming wearable, and consumer electronics are also transitioning towards healthcare applications. In recent years, consumer smartwatches have expanded their health monitoring features. Leading products in the market, such as Apple Watch and Samsung Galaxy Watch among others, have obtained FDA clearance and CE marking for their diagnostic abilities. These diagnostics hold promise in detecting silent diseases like hypertension and atrial fibrillation that enables early intervention and proactive healthcare measures.
Artificial Intelligence (AI) in Telemonitoring of Heart Failure
AI interprets complex data sets, aiding in diagnosing and preventing diseases like HF. Machine learning algorithms identify patterns in new data, continually refining treatment decisions. Moreover, AI allows the integration of data from various sources, where cardiological data is analyzed alongside data from other systems. It also reduces wait times, costs and enhances accessibility and patient experience.
Telemonitoring for Medication Adherence
Advanced software for processing and presenting adherence data could improve the acceptance and use of medication monitoring technologies. It has been found that the prevalent technology types, like electronic pill boxes or bags, and electronic pill bottles, rely on opening events to track medication ingestion. However, they face challenges such as pocket dosing and curiosity openings, which can affect the accuracy of adherence estimates. Despite these limitations, the popularity of developing pill monitoring devices persists, due to their discrete nature and ease of integration into patients’ daily routines.
The Economic Impact of Telemonitoring
One of the main drivers of telemonitoring is the cost-effectiveness it brings to the table. Human resources, the provision of appropriate technology, and the interactions between the medical team and patients are the main expenses of Heart Failure Telemedicine (HF TM). HF expenses typically represent 1–2% of total health costs in both the US and Europe, with hospitalizations, primarily due to hemodynamic congestion, accounting for over 80% of HF-related costs. Telemedical solutions have shown potential in reducing HF hospitalizations by about 30% through early congestion detection and correction, amounting to potential annual savings of approximately US$15.6 billion.
Multidisciplinary Care Teams
A multidisciplinary care team, comprising healthcare professionals like nurses, dietitians, primary care physicians, and administrators, works together to deliver high-quality, coordinated care. This approach is increasingly popular for managing chronic conditions and providing individualized care. A multidisciplinary team enhances patient care by providing comprehensive, specialized treatment that improves outcomes and satisfaction. Patients in such teams, particularly stroke units, have better survival and independence rates. This approach streamlines workflows, reduces errors and service duplication, and saves time, enhancing both patient and provider satisfaction.
How Can Empeek Help?
With our experience in developing real-time wireless medical monitoring software, HIPAA-compliant EHR system, and other medical apps and telemedicine software development services, we can create the needed telemonitoring solutions, customize and integrate them into your clinical management system. We know the importance of complying with the US standards and legal requirements of PHI collecting and data storage, and have expertise in working with US healthcare providers. Add to that a dedicated team of professionals and you get everything you need to change your approach to treating patients with heart failure.
End-to-End Development of Remote Cardiac Monitoring System with Wireless Heart Monitoring Device
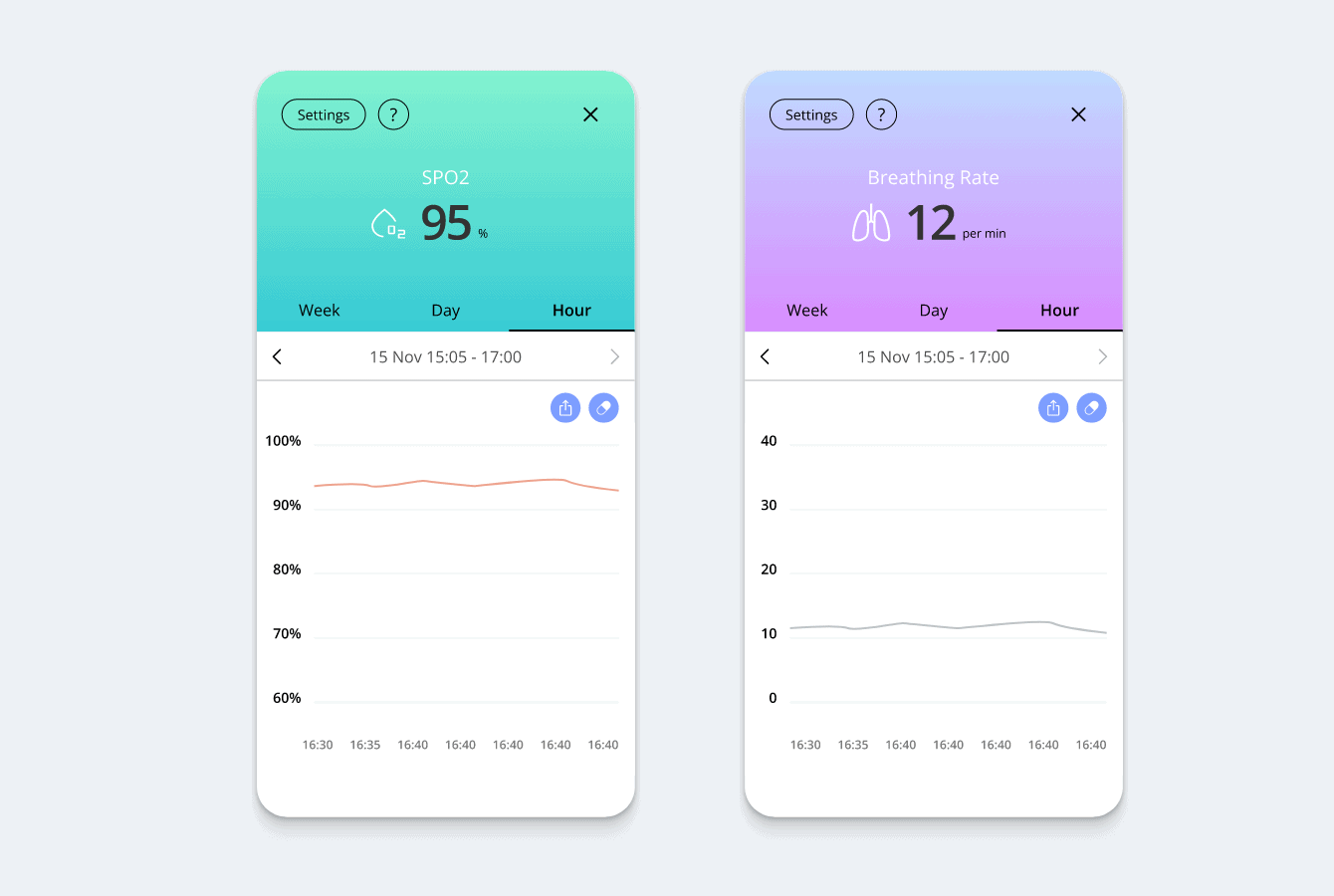
Empeek developed Remote Cardiac Monitoring System for our US-based client that provides a sophisticated solution for 24/7 cardiac health monitoring. This system sends real-time cardiac data to specialists who identify abnormalities. It tracks 5 health parameters: ECG, heart rate, SPO2, temperature and activity levels. The results are quickly forwarded to doctors for review, enabling informed medical decisions based on daily data fluctuations observed by both patients and doctors.
Patients use a compact, mobile ECG device from home that includes a patient diary feature for noting daily activities. An intelligent algorithm automatically filters and categorizes data, emphasizing high-risk abnormalities and alerting technicians to urgent cases. Our expert team developed a system that allows for customization, tailoring data collection to specific groups like athletes or children with differing heart rates, ensuring accuracy and relevance in monitoring.
BioBeat: Vital Sign Tracking In A Convenient Wearable Form
Empeek developed a remote patient monitoring system that is composed of an out of the box mobile app, custom wristwatch featuring PPG sensors and a cloud server. It securely transmits data to a cloud-based server accessible to patients and healthcare professionals by offering a solution that addresses both security and network availability concerns. Its key features are real-time data visualization, actionable alerts, medication reminders, fitness tracking and secure data storage.
The innovative system facilitates early detection of health issues and enables 24/7 remote patient monitoring. It’s scalable for monitoring unlimited patients, whether in hospitals or at home, and substantially reduces operational costs for healthcare providers. All ensuring compliance with HIPAA and GDPR regulations. The project has garnered CE mark approval and FDA clearance.
BioBeat uses MAX30100 Health Monitoring Sensor, which is an integrated pulse oximetry and heart rate monitoring solution that combines low-noise analog signal processing, two LEDs, a photodetector, and optimized optics. It enables smooth remote cardiac monitoring by conducting pulse oximetry and detecting heart-rate signals. It has gained interest in both research and clinical communities for early detection of cardiac health data based on photoplethysmogram (PPG) measurements.
Final Thoughts
It’s evident that the era of innovative telehealth solutions has arrived and offers patients exceptional medical care from afar. Telemonitoring fosters positive clinical results, increased patient satisfaction, and more robust health systems. The use of telemonitoring for the patients with heart failure is a growing trend in the healthcare industry that also shows plenty of benefits for patients, doctors, and hospital managers.
Using sensors, apps, and software to monitor physiological parameters regularly reduces urgent readmissions, manages workflow, predicts crisis intervention, and enhances the quality of care for HF patients. Empeek team is here to provide a customized telemonitoring solution that will improve your clients’ experience with your business and add value to the services you offer.








