Looking for a healthcare software development guide? This is the blog post by Alex Shpachuk, Empeek CEO, about how to develop healthcare software. We have interviewed Alex and now share the key insights to take you through the software development process, timelines, and estimates.
“I’ve spent years working at the intersection of healthcare and technology, and if there’s one thing I know for sure that the future of healthcare is all about smart and scalable software. According to HG’s data, the U.S. healthcare IT market includes 285,117 companies actively investing in digital solutions.
Innovation isn’t optional anymore, it’s expected. I saw how the right software can revive businesses, revolutionize care, and save lives. Building great healthcare requires a deep knowledge of compliance, user needs, and the complex machinery behind medical systems.”
What Differentiates Healthcare Software Development From Other Domains
In most industries, a software bug is an inconvenience. In the healthcare software industry, it can mean death. This space needs precision and airtight compliance. The landscape is massive and still growing, with research saying there are anywhere from 54,000 to 350,000 mobile health apps alone.
But volume doesn’t equal simplicity. Behind every app is a maze of regulatory hurdles, integration issues, and data locked in formats that were never meant to be read by machines. Here’s exactly what is different about healthcare software and why building for this field means playing by a very different set of rules.
Regulatory Limitations
Regulatory limitations in software development in healthcare in the U.S. are non-negotiable. HIPAA, for example, dictates how patient data must be protected, shared, and stored. Failure to comply results in severe penalties. For instance, in 2024, the Office for Civil Rights (OCR) took 22 enforcement actions, collectively resulting in $12.8 million in fines. In 2025, Oregon Health & Science University faced a $200,000 penalty after failing to provide one patient with timely access to their medical records.
Healthcare software compliance is vital for avoiding devastating financial and reputational consequences and is much stricter than in most other fields.
Learn more about compliance in Healthcare Software Compliance Guide
Issue of Unstructured Data In Healthcare
Everyday doctors scribble notes and nurses do verbal handoffs, adding scanned PDFs of handwritten forms. 81% of this critical data remains unstructured.
As a result, 32% of patients face gaps in care when records vanish between systems, and 1 in 20 endure repeated tests because their prior results are lost. Add the fact that medical records must be preserved for decades, but tech stacks evolve every few years. That’s a big challenge of software development for healthcare. Developers must tackle this chaos with tools like NLP for parsing clinical jargon and FHIR for breaking down data silos. This alone is a massive piece of work.
Importance of Integration and Collaboration
The variety of tools to integrate and align makes hospital software development a unique niche. Healthcare software must connect with legacy EHRs, lab systems, and medical devices, often with incompatible data formats. Bidirectional compatibility is essential because critical information may get trapped in unstructured formats.
Epic alone offers over 1,000 public API specifications to help bridge these gaps, but integration remains a major challenge. If software can’t sync with systems there are duplicate tests, delayed treatments, and preventable errors. To handle it, you must build healthcare software for interoperability from the start.
Complex User Interfaces
Healthcare software must serve clinicians who need to move quickly, but often forces them through complex menus and endless clicks. Studies show clinicians ignore up to 90% of warnings simply because there are too many notifications. Usually, systems bombard doctors and nurses with constant pop-ups so critical warnings get lost. In a survey of 2,067 physicians, 26.3% were dissatisfied with the readability of their EHR system.
However, delays and missed notifications because of poor UI/UX may cost someone life.
That’s why interfaces in medical apps must adapt to workflows, prioritize truly urgent alerts, and minimize unnecessary interruptions.
Data Monetization Barriers in Healthcare
Unlike social media platforms that trade in clicks, health systems can’t monetize records without explicit, revocable consent. And even then, the risks outweigh the rewards.
Anonymization sounds like a fix until you realize that 87% of Americans can be re-identified from just ZIP code, birthdate, and gender. That’s why HIPAA demands techniques like differential privacy, which adds statistical noise to datasets. Healthcare operates on razor-thin margins (hospitals average just 2-3% net profit), making costly privacy measures harder to justify. GoodRx was fined $1.5M for unlawfully sharing patients’ prescription data with ad tech firms like Google, Meta, and Twilio.
Main Types of Healthcare Software
When you look at the list of possible healthcare apps, you will see dozens of software types built to solve very specific problems. Some are there to keep hospitals running smoothly. Others improve how doctors treat patients or how people access care from home. To build something truly useful, healthcare software development companies must understand what each system is meant to do, how it works, and who it’s built for.
To make smart decisions with software development for the healthcare industry, always start by breaking things down. So, this section of the healthcare software development guide walks you through the main types of healthcare software.
| What for | Key features | Primary Users | Examples | |
| EMR/EHR | Stores and manages patient medical records | Patient history, prescriptions, lab results, secure access | Physicians, nurses, admin staff | Epic, Cerner, Allscripts |
| Hospital Management Software | Manages hospital operations and resources | Bed management, scheduling, billing, reporting, HR | Hospital administrators, staff | Meditech, McKesson |
| CDSS Systems | Assists in clinical decision-making | Alerts, diagnostic support, treatment recommendations | Doctors, clinicians | IBM Watson Health, UpToDate, Isabel. |
| HIM Systems | Manages health information and documentation | Data encryption, audit trails, reporting, HIPAA compliance. | Health information managers, coders. | MModal, 3M Health Information Systems. |
| Medical Billing Software | Handles patient billing and insurance claims | Claims submission, payment tracking, denial management. | Billing specialists, insurers, financial admins | Kareo, AdvancedMD |
| Telemedicine Software | Enables remote consultations and virtual healthcare services. | Video calls, e-prescriptions, patient portals. | Physicians, therapists, patients | Teladoc, Amwell, Doxy.me, Revive Telehealth, Vello Health |
| Laboratory Management Systems | Manages lab workflows and test results | Test ordering, result reporting, inventory control. | Lab technicians, pathologists | LabWare, STARLIMS, Applicant Information |
| Pharmacy Management Apps | Manages prescriptions, inventory, and compliance | Drug interactions, refill reminders, billing integration. | Pharmacists, pharmacy staff. | RxNT, PioneerRx, PharmASSIST. |
| Software for Medical Devices | Operation and management of data from medical hardware | Device integration, real-time monitoring, data export | Clinicians, biomedical engineers | Philips IntelliVue, GE Healthcare, BioBit |
| Health and Wellness Apps | Improve patients and users behaviour | Habit tracking, surveys, sleep tracking and others | Patients and users | Moodlifters, Endel, Asana Rebel |
Each software app has a specific purpose, from managing data behind the scenes to connecting patients with doctors in real time. When we build or evaluate a solution, we use features and goals breakdowns to focus on the core mission of custom software development for healthcare. Once we understand the landscape, we make better technical choices, avoid scope creep, and deliver real value to the people who count on it most.
Learn more about Top Healthcare Software Development Companies
Standards and Regulations That Affect Healthcare Software Development
Custom medical software development means you work within a complex framework of legal, ethical, and safety standards. These are requirements backed by real-world consequences, and they shape every decision from architecture to UX.
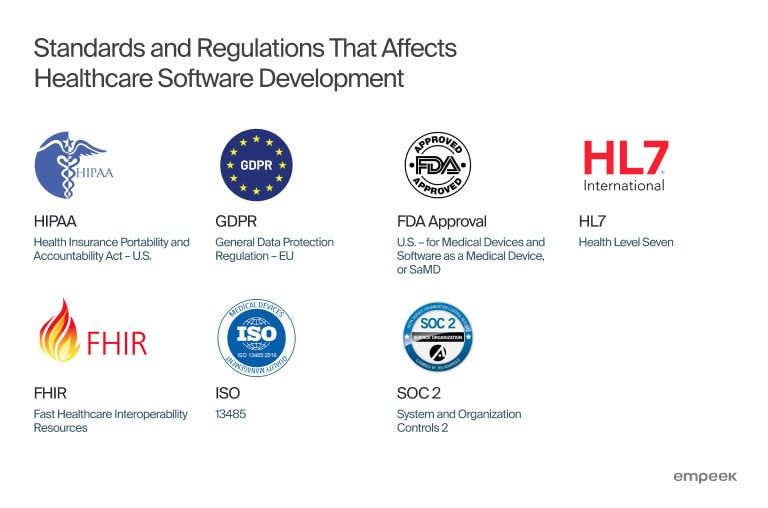
Here are the key regulations and standards Empeek’s team follows when building healthcare software:
- HIPAA (Health Insurance Portability and Accountability Act – U.S.)
Governs how healthcare organizations collect, store, and share protected health information (PHI). Requires strict access controls, encryption, and breach notification policies. (Learn more about HIPAA-compliant telemedicine software developemnt)
- GDPR (General Data Protection Regulation – EU)
Applies if your software targets users in the European Union. Focuses on data privacy, user consent, the right to be forgotten, and secure processing of personal health data.
- FDA Approval (U.S. – for Medical Devices and Software as a Medical Device, or SaMD)
If your software is intended to diagnose, treat, or influence medical decisions, it may be classified as a medical device. In that case, it must go through FDA clearance or approval.
- HL7 (Health Level Seven)
A set of international standards for the exchange, integration, and retrieval of electronic health information. Essential for interoperability between systems like EHRs and labs. - FHIR (Fast Healthcare Interoperability Resources)
A newer standard developed by HL7. It simplifies data exchange using modern web technologies like RESTful APIs. Widely adopted for enabling app integration in healthcare.
- ISO 13485
An international standard that outlines requirements for a quality management system (QMS) for designing and producing medical devices, including software.
- SOC 2 (System and Organization Controls 2)
While not healthcare-specific, SOC 2 is often required to prove your software meets strict standards for data security, availability, and confidentiality—especially when hosting sensitive health data.
How to Build a Healthcare App? 9 Stages of Healthcare Software Development
With custom medical systems software, every decision, from planning to deployment, must align with patient safety, compliance standards, and business needs. There’s no room for shortcuts or vague assumptions.
In this chapter, we’ll walk you through the core stages of healthcare software development, and show how to move from idea to implementation with clarity and confidence.
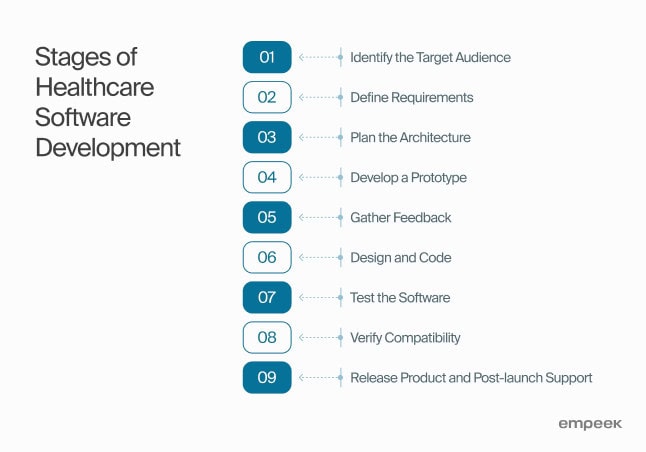
1. Identify the Target Audience
To serve 8 billion people with a single app is impossible. A solution that is meant for patients who manage chronic conditions, physicians in busy clinics, or administrators who are responsible for billing and compliance will be different. Defining the audience is the only way to craft something truly relevant. To skip this step is to waste time and money.
2. Define Requirements
At our healthcare software development company, we never start a new software project without going through a proper discovery phase. It’s our core recommendation on how to build a healthcare app that pays off.
At this stage, business analysts and other tech experts work with stakeholders to define the problems, understand the users, map the workflows, and assess technical and regulatory requirements.
A project focused on legacy system modernization for telemedicine company will have a very different discovery process than building an MVP from scratch. Modernization would require deep technical audits, data migration plans, and stakeholder interviews across departments.
MVP discovery, on the other hand, usually leans into rapid prototyping, identifying core features, and validating assumptions. Each format is tailored to the project’s context, goals, and constraints.
With the right investment in discovery, we can reduce development costs by up to 30%. It helps expose hidden risks, eliminate unnecessary features, and align everyone around a shared vision.
Reach out to the Empeek team, and we will provide a free consultation on your project.
3. Plan the Architecture
At this point, you must bring in solution architects, tech leads, DevOps engineers, backend healthcare software developers, and security experts to define how every system component fits together. Each person covers different aspects, like how to scale the system, secure patient data, ensure uptime, and integrate with existing tools. A well-planned architecture helps the team move faster later, avoid expensive rework, and make hospital software development compliant.
4. Develop a Prototype
Once we have an architecture and understand the core user needs, you can move on to building a prototype. This can mean clickable wireframes, a simple front-end demo, or a stripped-down version of a key feature. We work closely with designers, product managers, and sometimes clinicians to make sure the prototype reflects real use cases, not just what looks good on paper. A prototype gives stakeholders a rough app version. Also, it’s one of the fastest ways to spot flaws early.
5. Gather Feedback
Your next step is to gather feedback and test assumptions before further investing in software development for medical organizations. Now we want to know what works, what doesn’t, and what feels confusing or unnecessary. Set up sessions with patients, doctors, nurses, and admins, whoever the end users are and observe how they interact with the prototype. You can also rely on product managers, UX researchers, and QA testers to help collect insights, document issues, and prioritize improvements.
6. Design and Code
The healthcare software design process needs UX/UI designers, product managers, and healthcare staff teamwork. It’s important to meet user needs and make the interface intuitive. The development team of frontend engineers and backend developers then takes these medical software designs and begins coding to write secure and scalable code that manages complex tasks.
7. Test the Software
Testers join the project as soon as the functional software parts become available and keep testing software during the whole process. Manual testing often works in the early stages of a new healthcare app, but automated testing is needed for larger, more complex systems. For instance, when updating an old system, where many processes are already documented and stable, automated testing becomes invaluable. Automated tests save time and money by testing large parts of the software repeatedly without delaying new releases.
8. Verify Compatibility
Healthcare software rarely works on its own. It often needs to communicate with third-party tools, from HIPAA-compliant messaging systems to geo-location modules, external scheduling platforms, and popular EHR systems like Allscripts, EPIC, or Cerner.
So compatibility verification means testing for easy data transfer, checking compliance with the necessary standards, and verification that all integrations work as intended.
9. Release Product and Support It Post-Launch
Once the software passes all tests and compatibility reviews, it’s time to release the product to users. As users share their thoughts, you must continue to improve the software to stay competitive. It means new features, interface changes, and occasional bug fixing.
A strong post-launch support strategy makes sure the product stays reliable, scalable, and ready to meet the evolving industry demands. Maintenance is an ongoing stage of the SDLC in healthcare.
How We Helped a Next-Gen Biotech Company Reinvent Its Digital Experience
One of the most exciting projects we’ve recently scoped involved a biotech company specializing in medical devices and biological innovations. Their request was:
“We are looking to revamp our healthcare presence to better reflect our identity as a next-generation, cutting-edge biological and medical device company. Our goal is to create a visually compelling, modern, and highly functional system and website that showcases our innovation, expertise, and leadership in the biotech space.”
Here is how we approached this type of healthcare software project, including methodology, key phases, and the important questions clients must answer to ensure a successful launch. Check this part of the healthcare software development guide to better understand how to build a healthcare app and what information you must have at the project start.
Key Questions We Asked the Client
Business Goals and Identity
- What specific aspects of your innovation and expertise do you want to highlight?
- Who are your primary target audiences (patients, healthcare providers, investors, researchers)?
- What are your key differentiators from competitors?
- What is your 3-5 year business vision, and how should the digital solutions support it?
Current Systems Analysis
- What systems are currently in use and what are their limitations?
- What data and functionalities need to be migrated to the new system?
- What integration requirements exist with other systems or partners?
- What are the current pain points for users and administrators?
Feature Requirements
- What specific features are essential for your website and healthcare system?
- Do you need patient/customer portals or dashboards?
- What research data or results need to be showcased?
- What level of content management capabilities do you require?
- Are there specific regulatory compliance requirements to address?
Technical Considerations
- What are your hosting preferences and security requirements?
- What analytics and reporting capabilities do you need?
- What is your approach to data privacy and protection?
- Do you need mobile applications in addition to web platforms?
Project Parameters
- What is your budget range for this project?
- What is your desired timeline for implementation?
- Who will be the key stakeholders involved in the project?
- How will success be measured for this revamp?
Proposed Approach for Healthcare Software Product Development for BioTech
Phase 1: Discovery & Strategy (4-6 weeks)
- Stakeholder interviews and requirements gathering
- Competitive analysis of biotech/medtech digital presence
- User research (internal teams, partners, potential clients)
- Content audit and information architecture planning
- Technology stack evaluation
- Brand identity alignment workshop
Phase 2: Design & Prototyping (6-8 weeks)
- Visual identity refinement (color schemes, typography, imagery style)
- UI/UX design for both web and healthcare system interfaces
- Interactive prototypes for key user flows
- Design system creation for consistency
- Accessibility compliance planning
- Medical device/regulatory compliance review
Phase 3: Development (12-16 weeks)
- Frontend development (React/Vue.js for website)
- Backend development (Node.js/Django for system)
- Mobile development (React Native, Swift, Kotlin)
- Database architecture (PostgreSQL/MongoDB)
- API development for system integrations
- EHR/EMR integration if needed
- Security implementation (HIPAA/GDPR compliance)
- Content management system implementation
Phase 4: Testing & QA (4-6 weeks)
- Functional testing
- Security testing and penetration testing
- Performance testing
- User acceptance testing (UAT)
- Accessibility testing
- Cross-browser/device testing
- Compliance validation
Phase 5: Deployment & Launch (2-4 weeks)
- Staging environment final review
- Phased rollout strategy
- Training for internal teams
- Documentation completion
- Go-live support
Phase 6: Post-Launch & Optimization (Ongoing)
- Analytics implementation
- Performance monitoring
- Continuous improvement cycle
- Content updates
- Feature enhancements
Approximate time and budget estimates for the project
| Phase | Timeline | Cost Range | Key Deliverables |
| Discovery & Strategy | 4-6 weeks | 15k−30k | Requirements doc, sitemap, tech plan |
| Design & Prototyping | 6-8 weeks | 25k−50k | UI designs, prototypes, design system |
| Development | 12-16 weeks | 80k−150k | Functional system, website backend |
| Testing & QA | 4-6 weeks | 20k−40k | Test reports, compliance docs |
| Deployment | 2-4 weeks | 10k−20k | Live environment, training |
| Post-Launch Support | 6-12 months | 15k−30k/yr | Maintenance, updates |
Total Estimated Range: 165k−320k (excluding ongoing costs)
What Clients Often Underestimate (And How to Avoid It)
From years of working in healthcare tech, here are common challenges clients face and how to plan around them:
| Challenge | Why It Matters | Tip |
| Unclear Vision | Without a focused story, design becomes vague or generic | Align on brand narrative and audience before design |
| Compliance Complexity | HIPAA/GDPR oversights can cause major delays | Involve legal/compliance teams early in the process |
| Slow Review Cycles | Approvals from multiple departments can stall timelines | Assign a single internal project lead for decisions |
| Underestimating Content Needs | Even with a CMS, writing and structuring biotech content takes time | Start content planning in parallel with design |
| No Long-Term Plan | Websites need iteration—especially in biotech | Set up analytics + a post-launch roadmap for updates |
Cost of Healthcare Software Development and What May Increase It
The cost of healthcare software development depends on the system’s complexity, features, integrations, compliance requirements, and ongoing maintenance. Below is a rough breakdown of cost ranges for different types of healthcare software based on industry benchmarks and our experience at Empeek.
| Type of Software | Estimated Development Cost | Typical Complexities That Add Cost |
| EMR/EHR | $205,000 – $1.5M | Complex workflows, strict compliance (HIPAA, HL7), legacy system integration, role-based access |
| Hospital Management Software | $164,000 – $1M | Bed/resource tracking, multi-department coordination, real-time data syncing |
| Management Software | $123,000 – $800,000 | HR modules, billing integration, scheduling engines, performance dashboards |
| CDSS Systems | $246,000 – $2M | AI-driven recommendations, data science/ML integration, real-time EHR syncing |
| HIM Systems | $123,000 – $700,000 | Audit trail creation, HIPAA compliance automation, complex reporting features |
| Medical Billing Software | $82,000 – $500,000 | Insurance provider integrations, claims processing logic, denial management workflows |
| Telemedicine Software | $61,500 – $400,000 | Secure video/audio, e-prescriptions, real-time patient record sharing, cross-device compatibility |
| Laboratory Management Systems | $102,500 – $600,000 | Lab device integration, test result automation, multi-location support |
| Pharmacy Management Apps | $82,000 – $600,000 | Drug interaction checkers, compliance tracking, POS system integration |
| Software for Medical Devices | $205,000 – $2M+ | Real-time hardware integration, device certification, FDA/CE compliance, telemetry features |
| Fitness and Wellness Apps | $41,000 – $300,000 | Wearable integration, personalized analytics, habit-tracking algorithms, gamification |
Trends and Innovations in Healthcare Software Development
The healthcare industry doesn’t move fast for the sake of novelty. So when the technologies show real promise, they’re worth paying attention to. Some medtech trends fade out quickly. Other new technologies in healthcare reshape the way care is delivered, data is handled, or users interact with systems.
This chapter reviews five trends and new technology in healthcare that are actually making a difference. The ones you can see in real projects, real hospitals, and real patient outcomes.
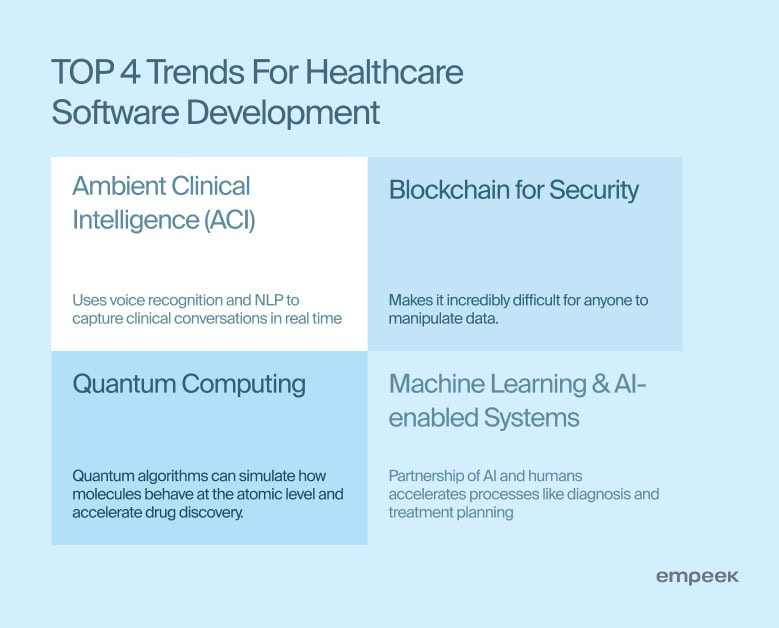
Ambient Clinical Intelligence (ACI)
At its core, ACI uses AI-powered tools like voice recognition and natural language processing to capture clinical conversations in real time. The standout example is Nuance DAX. This solution, used with patient consent, captures conversations during exams or virtual visits and processes them using AI to generate detailed clinical documentation. It removes the need for manual note-taking without disrupting the clinical flow.
In particular, at WellSpan Health, the introduction of DAX led to a noticeable shift:
- 97% of patients said their physicians were more focused, personable, and engaged
- 80% of physicians reported they could see more patients
- Average wait times dropped by 9 minutes
Blockchain for Security
Blockchain offers practical ways to secure healthcare data and increase trust in digital systems. Its decentralized nature makes it incredibly difficult for anyone to manipulate data. That’s critical in a space where privacy breaches cost millions of dollars each year and result in closed businesses.
In 2021, a study published in the Journal of Medical Systems found that blockchain-based frameworks improved data integrity and traceability in clinical trials by up to 95%, drastically reducing errors in recordkeeping.
BurstIQ, for example, provides a blockchain-based platform that manages health data with secure sharing between patients, providers, and researchers, enabling full data ownership and compliance. Another player, Guardtime, developed a blockchain system for securing medical records and tracking changes in real time, which is used at the national level, including Estonia’s digital health infrastructure.
Quantum Computing
Quantum computing still feels sci-fi. Unlike classical computers, which process information in bits, quantum systems use qubits to perform complex calculations at speeds we couldn’t imagine just a few years ago.
In drug discovery, quantum algorithms can simulate how molecules behave at the atomic level, something that would take traditional computers months or even years.
IBM, for example, is working with healthcare organizations through its IBM Quantum platform to speed up molecule simulation and shorten R&D cycles.
Another player, D-Wave, partners with pharma companies like GlaxoSmithKline to accelerate drug discovery.
For organizations looking to stay ahead in research, diagnostics, or drug development, quantum computing is something to keep a very close eye on.
Machine Learning and AI-enabled Systems
Artificial Intelligence (AI) and Machine Learning (ML) are here to stay, and their influence will only deepen as they continue to evolve. AI serves as an augmentation, not a replacement, for human expertise. Healthcare professionals remain responsible to make sure that AI-driven insights are interpreted correctly and applied ethically.
No one is willing to delegate critical decisions entirely to machines. This partnership accelerates processes like diagnosis and treatment planning that lead to healthier populations and better margins.
According to a report by McKinsey, approximately 50% of healthcare organizations have implemented AI in at least one function, with expectations of increased integration in the near future. This growth has been accelerated by federated learning (FL) that allows multiple healthcare institutions to collaboratively train machine learning models without sharing sensitive patient data.
Conclusion
After covering all the steps of the healthcare software development guide, Alex Shpachuk, Empeek CEO, summarized:
“We’ve built, scaled, and fixed more healthcare products than I can count. Some launched fast. Others needed time to get it right. Every decision, from the first lines of code to final compliance checks, has the potential to shape lives.“
You might be building an MVP or modernizing a legacy system, this guide has walked you through what it takes to develop impactful solutions in this field. From understanding regulations like HIPAA and FHIR to embracing the power of AI, blockchain, or quantum computing, success depends on the right mix of innovation, discipline, and empathy.
Contact Empeek for consulting or software development help. We can staff engineers for your ongoing project or develop custom software for healthcare management from scratch.








