The healthcare industry is rapidly adopting mobile technology and shifting towards electronic health record (EHR) platforms that can be accessed on smartphones and tablets. According to the Office of the National Coordinator for Health Information Technology (ONC) in 2021, approximately 78% of office-based physicians and virtually all non-federal acute care hospitals had implemented a certified EHR. This signifies significant progress over the past decade, considering that in 2011, only 28% of hospitals and 34% of physicians had adopted an EHR.
Mobile EHR apps are purpose-built to boost clinician productivity, coordinate care between various providers, and increase patient engagement outside the walls of the medical facility. The research found that physicians spend 44,9% of their total time (excluding Personal Time) on EHR data entry alone, so mobile access can greatly improve efficiency (Annals of Internal Medicine).
By providing easy access to medical data and decision support tools, mobile EHR apps enable clinicians to deliver more responsive care on-the-go. Intelligent alerts can coordinate entire care teams and prompt critical actions even when away from the office or hospital. According to the research, 64% of nurses reported improved coordination of care with the use of mobile healthcare apps.
User-friendly mobile interfaces also enhance patient transparency and self-management by allowing tasks like appointment scheduling, prescription refill requests, payments, and easy access to their own electronic medical records. Based on the research, up to 53% of patients expressed interest in using mobile apps to engage in their healthcare. With mobile EHR technology, patients become more informed and involved in their own healthcare.
Best practices for developing mobile EHR software focus on adapting to real-world clinical workflows rather than forcing desktop interfaces onto a mobile device. When thoughtfully implemented, mobile EHR apps have the potential to greatly improve clinical efficiency, care coordination, patient satisfaction, and health outcomes. However, mobile access also raises new security considerations that must be adequately addressed to ensure protection of sensitive medical data.
Key Takeaways
- EHR systems are becoming widely adopted, with 78% of physicians and most hospitals now using them. This allows clinicians to access medical records and make better care decisions.
- Mobile EHR apps transform clinician workflows through alerts. They also use streamlined order entry, documentation, and decision support tools. In a study, barcode implementation decreased medication error risk by up to 74.2%.
- Patient-facing mobile EHR capabilities drive engagement by providing appointment scheduling, prescription requests, payments, medical record access, and patient education.
- Security is critical for mobile EHRs. Encryption, access controls, compliance with regulations like HIPAA, and separation of work/personal data help safeguard sensitive patient information. Multi Factor authentication can block over 99.9% of account compromise attacks.
- Native mobile EHR apps can be customized to optimize clinical workflows. Yet, they must have more overhead to support many platforms. Commercial off-the-shelf solutions offer simpler integration, but may be less flexible. Android dominates the mobile OS market with an 85% share, while iOS lags at 14.7%.
Mobile Electronic Health Records Platform Options
Healthcare organizations have two main options for implementing mobile EHR capabilities: custom-developed native apps or commercial off-the-shelf solutions. Each approach has advantages and disadvantages that should be carefully evaluated.
Native Mobile EHR Applications
Native mobile EHR apps provide full access to device capabilities. They can be designed around specific clinical workflows instead of repurposing desktop interfaces. Data and functionality are stored locally, so this allows more reliable offline usage. Yet, supporting iOS and Android and their many OS versions requires extra overhead. It’s worth mentioning that Android dominates the mobile OS market with an 85% share, while iOS lags at 14.7%. The main reason is that iOS is limited to Apple devices, while various smartphone and tablet manufacturers use Android.
Commercial Off-the-Shelf Platforms for Mobile EHR Software
Commercial off-the-shelf (COTS) mobile EHR platforms like Epic, Cerner, and Allscripts offer pre-built tools and components. Still, they may provide less flexibility to optimize for specialized use cases. Custom development of mobile EHR apps gives more control to match required functionality and workflows but at a higher cost. Healthcare IT leaders, deciding on mobile EHR apps, need to weigh the advantages of purpose-built native apps against the simpler integration but possible drawbacks of COTS products.
Mobile EHR App for Clinician Workflow Optimization
A well-planned mobile EHR software delivers powerful capabilities. It transforms clinician workflows through targeted communications and assisted decision-making. Let’s see in more detail how it improves clinician workflow.
Alerts and Notifications
The mobile EHR apps enable push notifications for test findings, gaps in care, or simple reminders. Besides, care team members can coordinate smoothly through push notifications to align on updated protocols or care transitions.
In a study on a weight loss app for women, those who got push notifications lost more body fat and weight. This shows that reminders help people stick to their diet and exercise plans.
A cancer tool called Project Rōnin uses push notifications to remind patients to track symptoms between doctor visits. This clinical information on a patient’s health helps doctors make better treatment decisions using artificial intelligence, tailoring care to each patient.
Streamlined Order Entry and Documentation
Mobile EHR apps make it easy for healthcare providers to enter orders quickly by offering ready-made templates. This reduces the need for manual input and helps avoid errors. With streamlined order entry, providers can focus more on patient care and decision-making. Streamlined order entry can be achieved by scannable barcodes or voice dictation input.
Here is a quick guide to features that help to streamline order entry and documentation:
Templated Order Sets
Clinicians can select from pre-built order templates for common procedures and diagnoses rather than entering each order manually. Default selections reduce typing and chances for errors.
Voice Dictation
Speaking free-form notes or using voice commands to navigate orders and documentation is faster and more natural than typing on mobile devices. Voice input improves clinician efficiency and documentation quality.
Macro Shortcuts
Clinicians can define shorthand macros that expand into frequently used phrases or full order sets to skip repetitive typing. For example, typing “.diabetes” could expand into a full diabetes order panel.
Digital Signatures
Providers can sign off on documentation using digital signatures rather than printing forms. Signatures can be captured via stylus, touch, or other methods.
Revision Tracking
All changes to orders and documentation are logged and timestamped.This allows easily reviewing the revision history, changes, and by whom.
Data validation
Orders and documentation are validated against clinical rules to catch potential errors or inconsistencies for correction prior to finalization.
Optimized order entry and documentation functionalities help clinicians maximize time with patients while minimizing administrative burdens. Streamlining these frequent tasks improves clinician satisfaction, productivity, accuracy, and responsiveness.
Customization for Specialty Clinical Workflows
The system can be highly customizable across clinical roles. For example, diagnostic image viewing can be optimized for radiologists’ workflows. This can be done with easily accessible niche annotation and image analysis tools. Dentists can access tailored dental charting tools and procedure templates.
Embedded Protocols and Decision Support
Adding evidence-based guidance to healthcare systems boosts efficiency. Diagnostic decision trees are helpful guides for healthcare providers when patients show symptoms. They ask relevant questions and suggest steps to make diagnosing conditions easier. Using these embedded protocols and decision support tools gives healthcare professionals a more organized and efficient way to assess and diagnose patients. This speeds up the diagnosis and makes clinical decision-making more effective.
Diagnostic Decision Trees
- Suspected condition-specific flow charts prompt for patient symptoms.
- The flow charts are designed based on established clinical guidelines for appropriate diagnostics.
- Selecting a symptom like chest pain triggers recommended lab tests like cardiac enzyme panels. Or selecting shortness of breath prompts imaging tests like CT angiography to confirm diagnosis.
The clinical decision tree ensures clinicians don’t overlook diagnostic steps recommended in guidelines. This results in faster informed diagnosis following evidence-based standards of care.
Evidence-Based Order Sets
Custom order sets are configured to automatically populate appropriate diagnostic tests. These are programmed based on published guidelines for baseline testing by diagnosis. For example, a heart failure order set would include NT-proBNP, echocardiogram, EKG. The order sets reduce unnecessary repeats or redundant tests being ordered and minimizes errors of omission from an overloaded clinician missing something. The streamlined order sets enhance adherence to evidence-based care for each condition.
Differential Diagnosis
A mobile EHR algorithm suggests the most likely diagnoses based on symptoms entered. It cross-references a medical ontology against the patient’s symptoms profile. Then it prompts the clinician to rule out the most critical and time-sensitive conditions first. Before listing other potential diagnoses in order of likelihood. Then standardized treatment protocols are displayed to follow for the confirmed diagnosis. This supports clinicians sorting through the complex web of conditions connected to patient symptoms. And optimizes speed to definitive diagnosis and treatment.
Medication Recommenders
Once the patient’s final diagnosis is determined, the mobile EHR suggests medication options to consider. The recommendations are informed by the patient’s medical history, lab results, and potential drug interactions. It highlights relative out of pocket costs for each medication alternative. As well as alternatives in the same therapeutic drug class as options. Relevant warnings related to the patient’s kidney function or allergies are flagged. But the final prescriber decision on which medication to order is informed by this evidence-based guidance. Not determined by it categorically. This achieves personalized optimization of the patient’s drug therapy.
Mobile EHR Data Access
Mobile EHR systems liberate data from desktop constraints, providing on-demand access unbound from specific locations, while ensuring security. This facilitates responsive healthcare delivery and coordination by leveraging key features:
Lab Tests Results
Prompt diagnostics review is essential for critical care decisions. It helps with treatment escalation when needed. Mobile EHR allows doctors to configure alerts for abnormal lab test results when the lab populates the data. There is no need for physicians to make manual searches. Also, graphical trend analysis can make it easier to track values over time.
Smart representations such as flow sheets, graphs, or automated annotations go beyond static numbers, emphasizing relative risk bands. This aids clinicians in quickly interpreting significance at a glance. So, they can have swift comparisons against the patient’s previous baselines to determine whether a particular marker reflects acute changes or is chronically typical for their current status.
Physicians can immediately share lab findings through the mobile EHR app to close the loop.
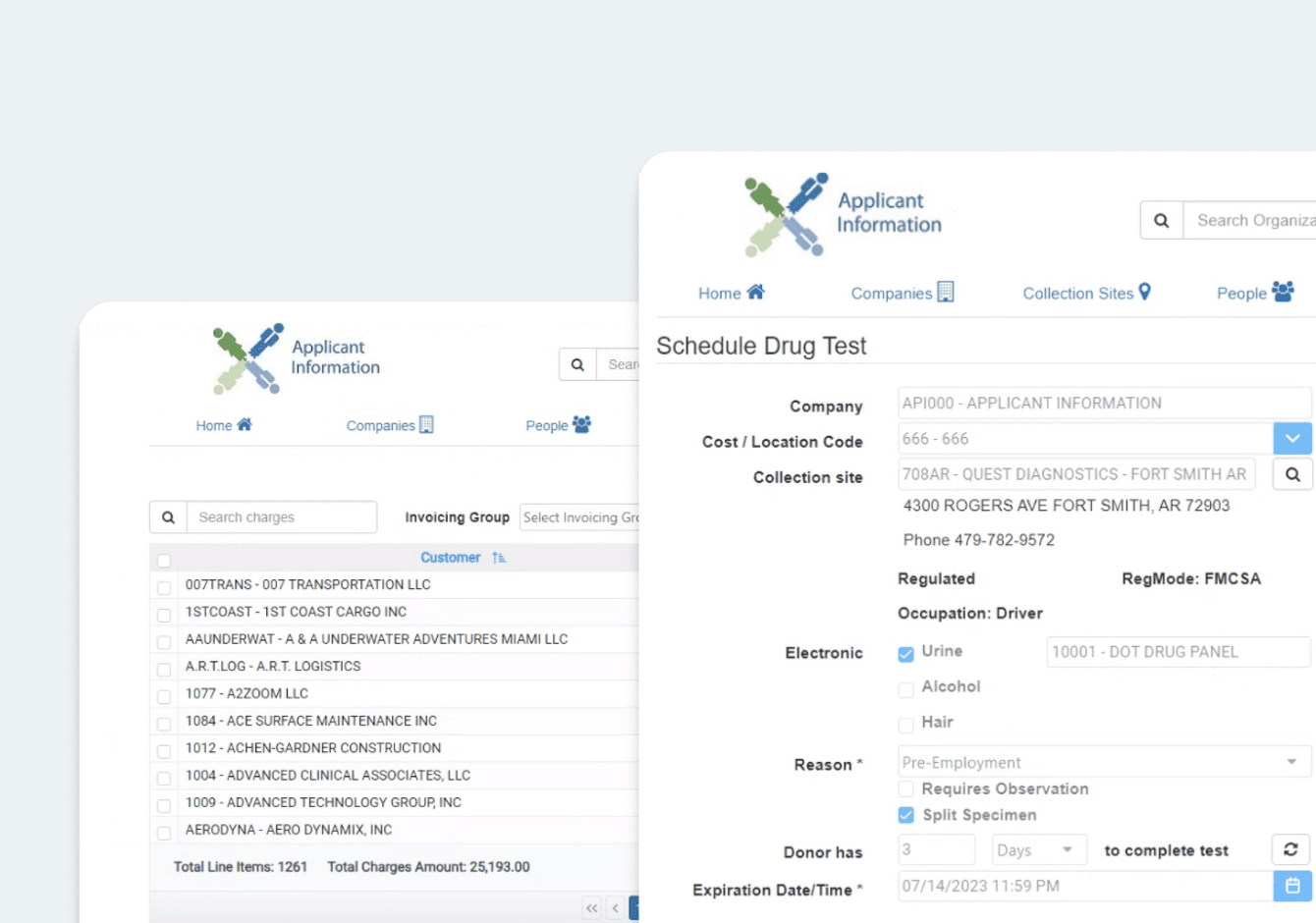
Read our case study: Lab Testing Platform for Managing, Tracking, And Accessing Drug Testing Data
Medical History Details
Consolidated clinical, family, and medication histories in graphical formats aid cognition. Timeline views relate key events such as diagnosed conditions, vitals, and lab trends. They are aggregated over the patient journey. Algorithms can analyze historical data. They suggest correlations or risk factors that influence new diagnoses or outcomes. It can also suggest correlations or risk factors influencing new diagnoses or outcomes.
For example, a patient who had normal blood pressure developed hypertension. An automated analysis could flag a 1–2 year switch to a steroid drug, which increases BP, as the possible cause. This would prompt confirmation and documentation of the link in the electronic health record.
Barcode Scanning
Scannable wristband ID barcodes auto-pull up electronic medical records for positive patient identification. NDC drug labels integrate into e-prescribing workflows, removing typing and potential erroneous selections. Supply cabinet inventories also use barcode tracking for billing reports and analytics. Barcode inputs verify patient identity and cross-check documented allergies against prescribed medications. This forms a safety net, avoiding overrides and allowing effortless adoption.
According to research, barcode implementation can decrease the medication error risk by up to 74.2%.
Offline Data Availability
Synchronized data enables reliable access regardless of connectivity disruptions. This is vital for on-the-move usage across service areas and remote locations. Caching ensures valuable information remains available, reducing workflow disruptions. Storing patient charts locally allows referencing recent vitals, medication history, and the latest physician or patient notes. It avoids relying on continuous signals.
Patient Engagement Features
While optimizing clinician-facing workflows is crucial, patient experiences equally impact health outcomes and must be addressed in tandem. Mobile EHR solutions are a prime channel for fostering engagement, transparency, and self-management of care. Features purpose-built around patient needs can connect consumers to their health data, care teams, and educational resources on convenient mobile platforms as part of daily life.
The mobile EHR software includes robust patient-centered tools. These include convenience functions like scheduling and integrated payments. It also has video patient encounters, wearables integration, education flows, and patient records. The solution aims to increase patient satisfaction and outcomes. It has four consumer-grade features.
Connected Patient Portal
The mobile EHR systems maintain a seamless connection with the provider-patient portal. Users can access their patient records, insurance details, yearly tests, scanned documents, care plans, lab results, and care team communications by logging into the connected portal. The portals or mobile apps updates are usually synced in real-time.
When people with diabetes use a patient portal, it helps them take better care of their health. A study by researchers at Kaiser Permanente found that those using a patient portal are likely to stick to their medications and manage their chronic condition more effectively.
Patient Education
According to the Agency for Healthcare Research and Quality, half of the patients leave their doctor’s appointments without fully understanding how to care for themselves. Also, patients and their caregivers often can’t remember much of the information that doctors share, ranging from 40% to 80%. That’s why patient education becomes a necessity.
Relevant patient education content is based on diagnosis or prescribed medications. Clinicians can share educational multimedia directly with patients via the EHR systems. Custom patient education handouts can also auto-populate drawings from condition-specific content libraries.
Patient-Reported Outcomes
Patient-reported outcome measures (PROMs) capture patients’ critical health and quality-of-life data. PROM platforms should incorporate validated instruments like EQ-5D and PROMIS to gather patient perspectives.
Patients can be prompted to complete standardized PROM questionnaires via EHR software at key points during treatment. These cover symptom relief, functional impacts, side effects, and overall health. Questions should be accessible across the mobile EHR systems.
PROMs present a more holistic view of therapeutic efficacy from the patient’s standpoint. For example, analyses may show gaps between clinical assessments reporting treatment gains and patient-reported outcomes. Dashboards can chart PROs and clinician-reported metrics together to reveal inconsistencies.
Flexible PROM frameworks also facilitate research and transparency. Standardized instruments enable projects to collect consistent outcomes’ data across patient cohorts. Reimbursement programs like MIPS use PROMs in value-based payment models tied to patient-centered outcomes.
The mobile EHR app aims to increase access, convenience, and clinical context. This helps to improve satisfaction and outcomes. It does so by providing a continuous patient engagement loop. This spans digital touchpoints before, during, and after a patient experience.
Security Considerations
Protecting highly sensitive patient health information is imperative when mobilizing clinical workflows outside a secure environment. This proposal bakes in state-of-the-art security, spanning four key areas — encrypting patient data in transit and at rest, identity and access practice management controls, adherence to healthcare regulatory compliance, and separating personal from work content on devices. Let’s explore them one by one.
Encryption of Data In Transit and At Rest
All mobile EHR data is secured while transmitting across networks and stored on devices. Protocols like SSL/TLS encrypt data-in-transit, and 256-bit AES encrypts data-at-rest. Encryption keys are also access-controlled. They use a secure key practice management solution for extra protection.
According to a recent survey, 68% of healthcare data breaches were due to lost or stolen devices. Yet encryption makes stolen data inaccessible without keys. According to IBM, encryption reduces breach costs by an average of $360,000.
Identity and Access Management
Permissions over patient information visibility are applied based on the user role. This limits access to only necessary patient information in the mobile EHR app. Clinicians only see patient data relevant to their specialty and job function. The system also supports biometric logins, such as facial or fingerprint recognition. These options confirm user identity securely.
One of the most advanced authentication methods is multifactor authentication (MFA). It’s a way to confirm a person’s identity by using at least two different things. For example, something they know (like a password), something they have (like a security token), or something they are (like a fingerprint). This helps ensure that the right person is logging in or doing something else that requires verification into the mobile EHR app.
Prove Identity’s 2023 State of MFA Report states that 61% of consumers enable MFA for mobile healthcare portals and mobile applications if they have this option. Moreover, according to Microsoft, MFA can block over 99.9% of account compromise attacks.
Compliance with Healthcare Data Regulations
Healthcare organizations must follow several strict data privacy and security regulations, with heavy penalties for non-compliance.
The key healthcare data compliance regulation in the United States is HIPAA (Health Insurance Portability and Accountability Act). It provides standards for protecting sensitive patient health information. Violations can result in fines of up to $1.5 million. The HITECH Act strengthened HIPAA compliance by increasing penalties. Other important regulations include GDPR (General Data Protection Regulation) in Europe, US state privacy laws, and industry-specific rules around proper data handling procedures.
EHR software solutions companies must build HIPAA-compliant software. Compliance violations from their systems can negatively impact customers. Healthcare providers can face huge fines, lawsuits, and loss of medical licenses. This can seriously damage an EHR software vendor’s reputation and finances. It can cause brand harm, loss of customers, and legal liability. Healthcare technology firms maintain rigorous data compliance. It assures customers that their systems will not lead to regulatory issues.
Separation from Personal Content
Enabling clinicians to access electronic health records on personal mobile devices (bring your device or BYOD) increases efficiency and poses compliance risks. Sensitive patient data could be mixed with personal content. Advanced mobile device management (MDM) capabilities can separate work and personal domains on BYOD devices.
Mobile EHR software data should be stored in a secure, encrypted container, isolated from personal apps or content. Containerization aligns with data protection regulations in health care. Strong authentication policies like biometrics or complex passwords can govern access to the container.
Selective wipe capabilities enable compliance for BYOD deployments. If a clinician leaves an organization, enterprise data in the container can be remotely wiped without deleting personal content.
Robust MDM solutions provide visibility into mobile EHR software access, permissions, and device-level policies. Centralized oversight, with detailed activity reporting, facilitates compliance audits for mobile environments.
These critical safeguards help ensure patient data stays protected on mobile devices. They also unlock the workflow efficiencies of mobility-based access.
Summing Up
Purpose-built mobile EHR apps boost clinician productivity and decision-making. These apps enable responsive, coordinated care and engage patients through user-friendly adoption.
An intelligent mobile platform acts as an electronic nervous system. It includes alerts, streamlined order entry, embedded protocols, robust security, and patient portals. This system connects care teams and delivers clinical tools to providers at the point of need. Providers can access these tools in clinics, at the bedside, or in patients’ homes.
This move from desktop workstations to mobile EHRs accommodates clinical demands. Thoughtful design ensures simplicity and efficiency for clinicians and brings transparency for patients.
The next-gen mobile EHR software promises gains through simplicity and efficiency for clinicians. It also promises gains for patient continuity and transparency. Creating an integrated ecosystem across care settings is crucial. It’s better than replicating legacy interfaces on mobile devices. This involves rethinking information needs beyond secure environments and leveraging mobile-native capabilities.





