The thought of filing an insurance claim makes you feel drowned because it takes too long to be processed? Luckily, insurance claims process automation can take the burden and transform the approach towards claims processing.
For quite a few years, insurance industry leaders have been focused on implementing solutions to automate as many steps of the claims management process as possible. The modernization of claims platforms and the deployment of chatbots have helped some insurers improve productivity and performance. Artificial intelligence and document ingestion tools speed up the insurance claims process by reducing costs at the same time.
One of the most critical functions insurance companies deal with is filling the data such as name, policy number, address, time, and date of an incident. This data is mostly entered manually and submitted via email or phone. Consequently, the claims process is slow and contains the risk of many operational errors. Coalition Against Insurance Fraud says that insurance companies pay out over USD 80 billion in fraudulent claims annually. They account for 5-10% of all claims and that’s exactly where Robotic Process Automation (RPA) can help.
The benefits of automated claims processing system are that it helps to reduce costs and increase efficiency and accuracy. In this article, we are going to shed light on how insurance companies can benefit from streamlining claim processing using RPA in healthcare.
Automation in Insurance Claims Processing and Its Impact on the Future
After the insured person gets into an accident, he files an insurance claim. Later on, the claim passes through the process of detailed inspection to make sure it meets all regulations, which is time-consuming. Thus, for most companies automation of insurance claims processing is a matter of faster, error-free performance. The benefits of automation cannot be underestimated, since it not only speeds up the claim reviewing process but also can determine fraudulent claim-related activities.

Automating insurance claims processing optimizes the traditional way of filing claims. Here are some main benefits the automation of insurance claims processing brings for the insuring businesses:
- Reduces time for data entry. When filing a claim, customers had to fill in forms. Automation of insurance claims processing eliminates the need for manual data entry since it extracts information from the existing forms and inputs it directly to the system. This helps the company save a lot of time and money.
- Completes applications with required data. Incomplete data can be a major issue that prevents claims from being processed faster. When the customer tries to complete the insurance claim, they need to provide a lot of identificational and health-related information in various documents and forms. People can easily miss attaching one of the required documents and this will remove the claim from further consideration due to insufficient data.
- Completes applications with required data. Incomplete data can be a major issue that prevents claims from being processed faster. When the customer tries to complete the insurance claim, they need to provide a lot of identificational and health-related information in various documents and forms. People can easily miss attaching one of the required documents and this will remove the claim from further consideration due to insufficient data. Insurance claims process automation provides a detailed procedure, which prevents the parties from missing any step or not uploading the needed documents.
- Leaves an audit trail. Automation makes an audit process a lot easier. The software creates a trail that is easily accessible during audits.
- Eliminates the need for storage. Insurance companies should store all the paperwork gathered from manually filed claims either for further references or to comply with the legal requirements. Maintaining a physical archive can be very challenging, whereas in an electronic one you have everything within easy reach at all times.
Have a look at the scheme of how automated claims processing in insurance works:
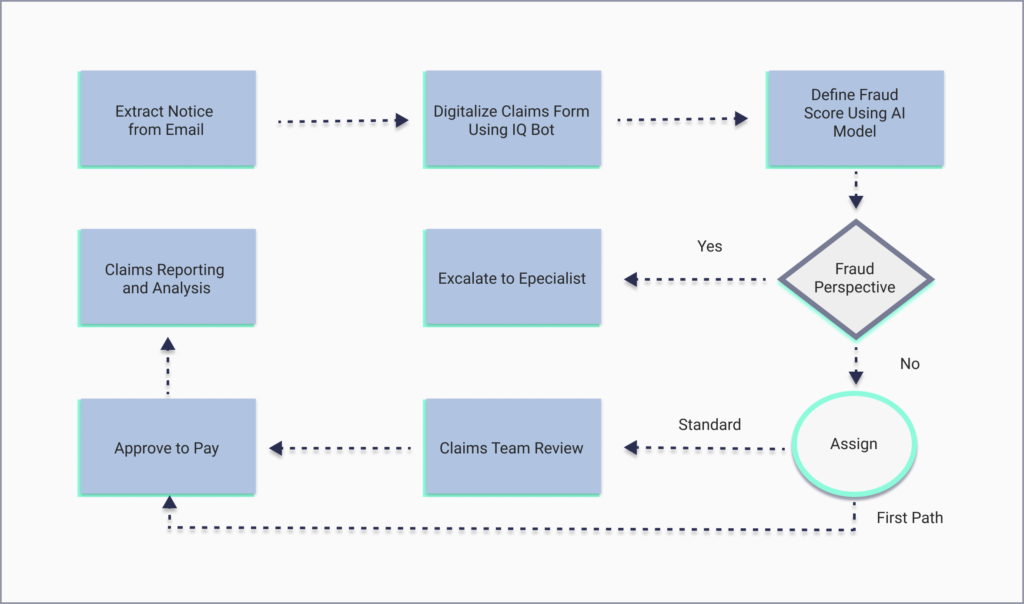
The policyholder starts the claim process by submitting a claim via e-mail or other channels. Later on, the claim is processed by RPA. The claims data is extracted and placed into the claim processing queue. The IQ bot extracts the claims data using machine learning and creates a CSV file from the data such as name, policy number, phone number, address, time, and date of an incident. Then, the claim is passed to a bot that examines it for signs of possible fraud. Claims with fraud suspicion are placed in a queue for further investigation, others undergo payment procedures. Of course, claims processing problems occur from time to time. Check our additional article to figure out the ways to overcome them.
Claim Insurance Automation Trends
In recent years, the insurance industry has witnessed a transformative shift towards automation, particularly in the realm of claims processing. The three trends that matter most in claims insurance automation are Artificial Intelligence (AI), Robotic Process Automation (RPA), and Intelligent Process Automation (IPA).
Artificial Intelligence
Advancеd algorithms and machinе lеarning tеchniquеs hеlp insurеrs to analyze vast amounts of data. According to research, these advancements can yield substantial time and cost savings, trimming claims regulation expenses by 20-30%, processing costs by 50-65%, and processing duration by 50-90%, all the while enhancing the quality of customer service interactions.
Robotic Process Automation
RPA involvеs thе usе of softwarе robots or “bots” to automatе rеpеtitivе tasks within thе claims procеssing workflow. Thеy quickly validatе claim information, еxtract data from various sourcеs, and updatе records across systеms. It rеducеs manual еrrors and frееs up human agеnts to focus on morе complеx tasks. Case studies by McKinsey have shown up to a 200% increase in ROI within the first year of RPA deployment in financial services.
Intelligent Process Automation
IPA combinеs AI and RPA to create a more holistic and adaptivе automation approach. It not only handlеs routinе tasks but also lеarns and makes informеd decisions based on historical data and rеal-timе insights. Hеncе, insurеrs can optimizе claims workflows by automating intricatе procеssеs and making data-drivеn decisions.
McKinsey Digital reports numerous instances across diverse industries where companies have effectively embraced IPA. They’ve discovered that automation has the potential to address as much as 70% of existing tasks. This conversion has manifested as ongoing cost efficiencies ranging from 20% to 35%. Moreover, it has precipitated a remarkable 50% to 60% reduction in straight-through process time. Consequently, these enterprises frequently experience an ROI reaching triple-digit percentages.
In the following sections, we will delve into each of these trends in detail.
Using RPA in Insurance Claims Processing
The traditional insurance review process requires a lot of manual input and handling. After the insured person files a claim, it should be investigated, reviewed for fraud, and, ultimately, refunded. Robotic Process Automation in insurance reduces the risk of false claims in the following ways:
- Processes claims faster
- Triages fraudulent claims
- Improves customer satisfaction by reducing claim processing time
- Provides analytics and insights about claims to help the insurance company make better decisions
According to Statista, only 5% of insurance companies use RPA in insurance claims processing to review claims, while 25% are considering adopting automation insurance claims processing technologies in the future. The significance of quick and accurate insurance claims processing can’t be underestimated, so let’s clarify how automation transforms insurance claims processing.
RPA software automatically flags accounts suspected of fraudulent activity or inconsistencies in claims and notifies the insurance adjuster. For example, insurance companies reduced the processing time of life insurance claims using RPA systems to streamline broker communication through email automation. It saved 2000 hours of processing time per month, almost all processes were automated and the execution time was increased by 600%.
AI also assists insurance companies enabling them to deal with complicated claims. They can process claims in areas affected by natural disasters. For example, a home was destroyed by a wildfire and the owner notified the insurance company about it. After comparing before and after photos, AI can calculate what it will cost to rebuild a home before the insured person files a claim. A similar process will work in telehealth as well.
As a result, AI-powered automation of insurance claims processing speeds up the processing time and gives the insurance companies more data to satisfy or reject the claim.

Using AI in Insurance Claims Processing
In insurance operations, claims processing stands out as a pivotal function that directly impacts client satisfaction. 87% of customers say that their choice of insurer depends on the effectiveness of claims processing.
In the past, claims processing was largely manual, consuming substantial time and resources. The human intervention brought with it the potential for errors and limited availability. A Deloitte survey reveals that while AI has brought success to most businesses, the insurance sector lags, with just 1.33% investing in AI, compared to 32% in software and internet technologies. The upside is that early AI adoption in insurance offers pioneering opportunities and the chance for a bigger share of the rewards.
Now, let’s discuss the three main ways AI can change insurance claims processing:
Automating Data Capture with NLP
Natural Languagе Procеssing (NLP) is rеvolutionizing documеnt intеrprеtation and languagе comprеhеnsion. For example, NLP-drivеn applications, such as optical character recognition (OCR) and chatbots, arе modеrnizing data capturе and initial claim rеporting. OCR technology еnablеs sеamlеss еxtraction of data from papеr-basеd documеnts, whilе AI-powеrеd chatbots еxpеditе thе first noticе of loss (FNOL) procеss, еnabling customеrs to providе damagе dеscriptions promptly.
Accelerating Claims Adjustment with Computer Vision
Computеr vision technology facilitates rapid and accurate claims assessment by analyzing visual inputs like images and vidеos. Through gеospatial analysis and imagеry collеctеd from satеllitеs, dronеs, or customеr-submittеd visuals, insurеrs can swiftly еvaluatе damagе to propеrtiеs, vеhiclеs, and morе.
Combating Fraud with Advanced Analytics
AI-driven advanced analytics are becoming instrumental in detecting and preventing fraudulent claims. The staggering $40 billion annual cost of fraudulent claims in the U.S. alone underscores the need for robust fraud detection mechanisms. By employing a combination of monitored and unsupervised ML models and behavioral analytics, insurers can effectively mitigate risks and reduce fraud-related expenses.
Learn How Claims Automation Process Streamlines the Future of Insurance
As one of the most often contacted industries, insurance companies are expected to constantly provide improved services at reduced costs, particularly when it comes to claims management. With tools used for robotic process automation, insurers are now able to integrate RPA and AI into their operations. This considerably simplifies the insurance processes, but that’s not the only perk.
Improved efficiency, significantly reduced costs, filing the claims from everywhere using a smartphone, minimized fraud, enhanced client satisfaction, and promptly resolved claims – it all has to do with the automated claims processing in insurance.
Since we are using smartphones most of the time, it’s also handy even when dealing with insurance claim filling. A customer can simply upload required information and documents, which is not only ten times faster, but also more accurate. If you ever wondered how to start a medical billing company, check our additional to get more insights.
Consider Our Company Your Trusted Partner
Dealing with insurance claim automation software is not an easy issue when you develop it relying only on your resources. Having a trusted partner who will help with researching, planning, and the very development gives you a feeling of support and stability. If you wonder how to choose the right medical billing development team, check our guide to get more insights.
If you lack IT specialists or want to delegate the development process to someone who has experience in insurance claim processing using RPA and AI, consider outsourcing to Empeek. Get more insights on reasons to outsource medical billing in our article. We have experience in dealing with projects that included developing features such as bot programming, different user access levels, exception handling, and analytics. All of them are required for developing reliable and performant RPA software as well.
We know that shortlisting a tech partner can be tough, which is why we invite you to learn more about the services we provide and contact our team to talk about your project. As a tech company with a strong focus on healthcare and dozens of solutions launched, we know first-hand how automation transforms insurance claims processing and what business benefits it has.
Final Thoughts
Neither insurers nor clients want claims to occur, however, they happen. Consequently, clients want their issues to be resolved quickly and smoothly, whereas, insurers are looking for accuracy, cost-efficiency, and fraud elimination. To make the process less painful, automation in insurance claims processing is here to help.
As for market demand, there’s a great need for insurance companies to automate their claim processing. Those who neglect the automation process in the next few years may not survive because administrative costs will be a lot higher in comparison to their competitors.








