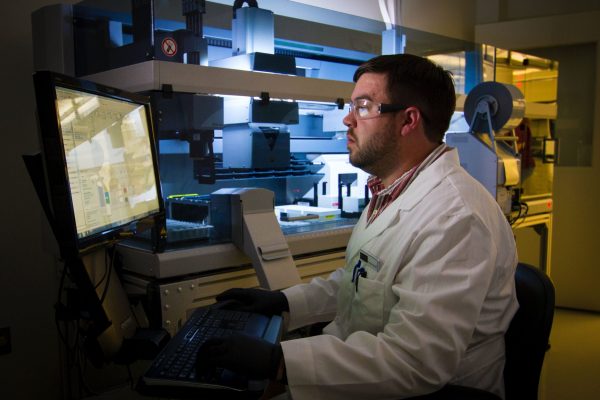
EHR integration is one of the key IT infrastructure priorities in healthcare, and failures during this process can be devastating to the overall medical practice’s performance. For one thing, the absence of electronic medical records slows down the administrative performance of the healthcare provider. For another, it prevents doctors from getting holistic information on patients’ health conditions, past treatments, and diseases to prevent medication misuse and erroneous interventions. Implementation of robust electronic health/medical records can help to avoid this negative experience. But how to do it the smart way by fitting in the budget and achieving the desired result on time?
In this article, we will guide you through the EHR system implementation process and share some best practices that will help you ensure EHR/EMR software development and deployment success.
What is the Implementation of the EHR System All About?
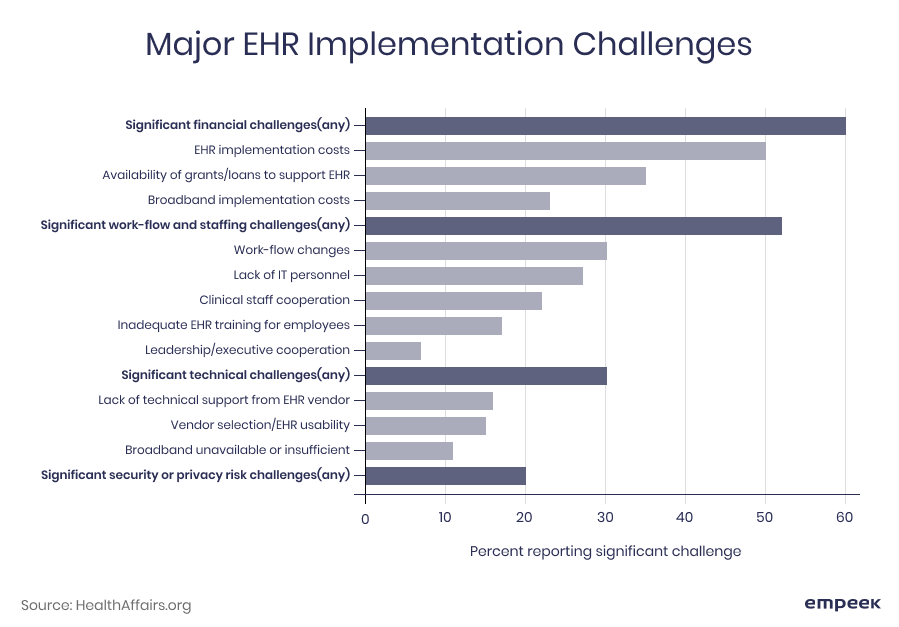
Like any technology adoption, the process of implementation of an EHR system is a complex, multistep process that requires a lot of preparatory work like creating the project plan, analyzing current organizational structure and processes, setting project milestones, choosing the integration method, and so on. As for EMR ROI, the research findings demonstrate that EMR software implementation and the adoption failure rate can reach up to 50% due to technical, organizational, or financial barriers along with ineffective strategy. The major EHR implementation challenges are displayed below.
Previously, electronic medical records were used to help doctors access patient data. Modern EHR/EMR systems go way beyond that. They streamline doctor-patient interactions, improve patient care, and provide secure, reliable, and accessible patient medical records storage available for any healthcare provider, and ensures patient check-in automated process. Therefore, if done right, implementing EHR will be beneficial for both patients and doctors.
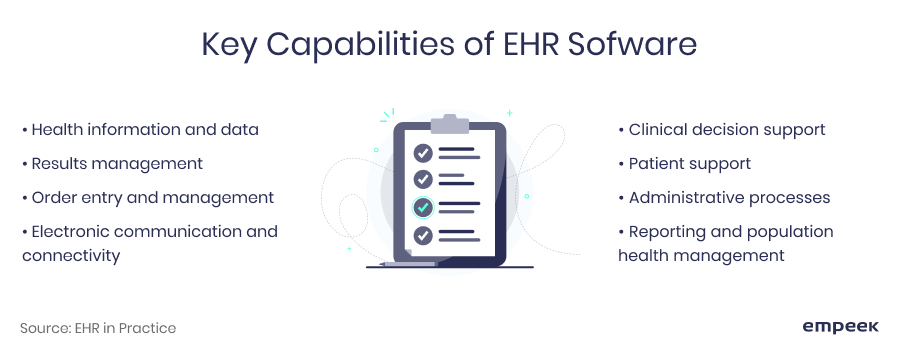
EHR systems vary in their complexity drastically, ranging from simple electronic data sharing tools to complex platforms for cross-functional alignment. That’s why it should be noted that various EHR and EMR software solutions will have different implementation life cycles.
The researchers state that typically an implementation of EHR takes 16 to 24 months from the decision-making moment till the system roll-out. However, accelerated EHR implementations can take from 6 to 12 months depending on the project scope. According to the Healthcare Information and Management Systems Society (HIMSS), there are 7 stages of EHR complexity, which are displayed below.
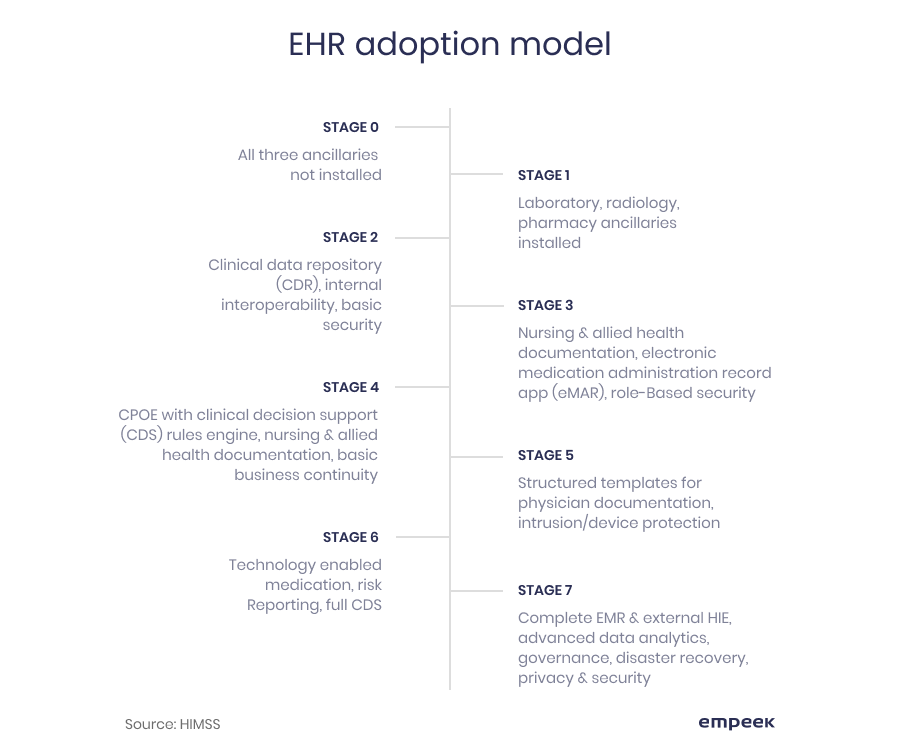
Figuring out how much time and resources it will take to implement EHR technology in healthcare is not a trivial task, and a wide range of the system’s capabilities and types of electronic health record systems makes it even more challenging. The question is, how to get it done successfully? Our advice would be to create a well-thought-out project roadmap with specific milestones, goals, and time estimates.
If you would like to get a more specific project estimate for your particular case, the best thing to do is to consult a team of experts. They will help you with setting realistic estimates of the desired system functionality regarding the timeframe and budget, which will not only save you from unexpected spending, but also will give a clear understanding of the process and what will be required along the way.
A Step-By-Step Approach to the EHR Implementation Process
To make sure that EHR/EMR implementation duration is optimal for your specific case, it is crucial to follow a well-thought-out implementation strategy. The question is, what do you need to know when planning EHR system implementation to make sure the process will bring you to the desired results within a certain time without breaking the bank? Well, we’ve got you covered with a comprehensive 11-stage guide that describes all the necessary stages of EHR implementation. Let’s go through them together.
Step 1. Conduct business analysis and set clear goals for EHR implementation
While business research might seem to be not quite connected with software implementation, we assure you EMR and EHR implementation success is heavily dependent on it. By taking a close look at current workflows and identifying data management or operational inefficiencies, healthcare organizations are able to plan the EHR software functionalities that would be most beneficial for a particular practice’s needs.
Step 2. Choose a reliable software development vendor and build your project team
An effective software vendor selection serves as a prerequisite to implementing an EMR system successfully. That is why it is vital to partner up with a trusted EHR development company that is able to dig deep into your business needs and provide you with software designed to solve your core operational problems.
A list of specific requirements or vendor evaluation matrix might come in handy at this stage. Some of the most common selection criteria are listed below.

Once your EHR implementation partner is selected, it’s time to specify the team roles and responsibilities of the parties. A close synergy between your staff and the vendor’s experts along with clearly defined roles is what makes a strong team. Usually, the EHR implementation team consists of the following members:
- Project Manager, who is responsible for establishing proper communication channels between your team and the EHR vendor. It may be your in-house expert or a specialist from a software vendor’s side.
- A physician champion and a team or medical assistant and nurse advocates, who are responsible for aligning business and IT needs.
- Business Analyst who takes care of identifying and specifying key requirements for the software based on one’s industry expertise. This role is commonly played by the company’s CEO, COO, tech executive, or dedicated in-house business analysts.
- Early system adopters who test out the system’s usability and define bottlenecks in user experience.
- Software developers who oversee the process of building the custom software and adding all the necessary features. Depending on the project scope, either one or several developers may work on the project.
- QA test engineer who checks the EHR system’s performance before the software roll-out.
- Data migration specialist who ensures a smooth transition between the legacy system and the new one.
Even though the roles listed above are the most common for a fully operational EHR implementation team, the projects having a large scope might require some additional members. Depending on a specific business need, organizations might also assign someone responsible for workflow redesign, billing process optimization, appointment scheduling and registration, and others.
Step 3. Create an EMR implementation plan
Implementation milestones, software development plan, the roadmap for EHR implementation – this stage might have different names, but all of them describe the same purpose: understanding how your perfect EHR/EMR system should look like.
At this point, it is crucial to identify success criteria for your project, plan the features set for your future software, agree on implementation costs, and set project deadlines together with a vendor. Also, it is high time to research government regulations and compliance standards, such as CCHIT and ONC-ATCB certification if the system is intended for use within the US, and review the ones of other countries in which the future EHR will be used.
Another thing to consider at this stage is the EHR system rollout method. For large-scale deployment, it might be a good idea to break down your software deployment process into several stages. You might also consider rolling out an MVP first. It is best to discuss all these aspects with your software development vendor who will help you out to opt for the best option in your specific case.
Step 4. Develop a communication strategy for optimized vendor relationships
A successful alignment between the key project stakeholders is one of the main factors for software’s timely deployment and successful EHR implementation. That is why you need to make sure a specific communication strategy is created and agreed upon with the entire team. The frequency of regular meetings, software development progress reports, and communication channels – all these aspects should be discussed beforehand and controlled strictly throughout the project.
Step 5. Pay attention to the layout and UX design
Designing a user-friendly and intuitive layout should be one of the key priorities when implementing an EHR system in healthcare. If done right, UI/UX design can improve both medical practitioners’ and patients’ experiences significantly. And since the positive user experiences with a new EHR/EMR system leads to betters business outcomes, don’t underestimate the importance of the user interface design.
Also, pay close attention to adaptive design best practices: believe it or not, the entire nature of the doctor-patient relationship and communication changes by introducing tablets, mobile-based solutions, and IoT devices.
Step 6. Get your IT infrastructure ready
Preparing your existing IT infrastructure for new software implementation is one of the most critical stages in the EHR implementation plan and it requires a thorough analysis of the existing technology landscape. Whether you get the proper hardware for your EHR system or deploy a cloud-based solution, make sure data interoperability will not be affected by the changes in your IT landscape. Otherwise, your overall operational efficiency might be at stake.
Step 7. Prepare for data migration
Transferring the old electronic health records to the new system is another important step. Data migration checklists prepared beforehand can be very useful. They will help you identify the scope of data that needs to be transferred, the sets of data that need to be excluded or deleted, and data conversions or transformations that must be done.
Also, don’t neglect to run several test scenarios with a set of users and compare the results with the same scenarios after the migration. It will ensure that the old data is intact and functioning properly.
Step 8. Perform system testing
Software testing might be a mundane and time-consuming stage, but it is crucial for EHR software implementation success. At this step, dedicated QA specialists will run the system tests to identify and fix software bugs and make your EHR solution more reliable and easier to use. Your role at this point is to monitor the process and ensure the services are delivered to you on time.
Step 9. Streamline user adoption with training sessions
To accelerate user adoption successfully, basic and advanced user training should be performed before a new EHR software goes live. It will make them feel more prepared for the change and even anticipate the new way of working. At this point, there’s no need to show them all the nooks and crannies of the new technology solution. Demonstrating basic and necessary functionality will be enough, and you will be able to catch up on the rest of it later on.
No training can be successful without a skillful trainer. Therefore, picking up someone from the team who can “sell” the idea of using new software is vital. The best thing to do is to pick someone from the project team since those who have been involved in the entire electronic health record implementation process make the most insightful and inspiring teachers.
Step 10. Always have a contingency plan in place
Of course, it is expected that the software you implemented is flawless and runs smoothly at all times. Nonetheless, even the most robust EHR software solutions have a certain level of malfunction risk. Embracing this fact and being ready with a backup plan in case it happens may help you avoid chaos and diminish negative effects instantly. That is why it is crucial to create a well-thought-out contingency plan and stick to it.
Step 11. Collect feedback for further software improvements
Last but not least, encourage your users to think of the ways the EHR system can run more efficiently. Finding navigation shortcuts, improving or adding some features, and perfecting the system’s UI/UX will be highly beneficial for user experience and bring better ROI in the long run. It’s also a good idea to keep in touch with your EHR vendor so you could upgrade the system from time to time and make it more efficient.
Top Tips for Successful EHR Implementation
There are quite a few barriers to implementing EHR systems. Here are some tips to make the transition to a new EHR system successful.
- The right partner is the key. Make sure you select a reliable software implementation vendor who understands your business needs well.
- Listen to your team, and not only decision-makers. Keeping the future system users engaged in the EHR or EMR implementation process may lead to gaining some valuable insights that would allow for designing a more efficient EHR solution.
- Don’t underestimate change management efforts. Winning the hearts of users who are reluctant to change might be harder than expected. That is why having a set of adoption strategies in place for your users is by far not less important than a software deployment itself.
- Remember that automation and optimization are not the same. A critical evaluation of organizational workflows will be required to tackle user experience challenges and design a new EHR software layout accordingly.
Challenges of Implementing The EHR System
While the benefits of EHRs are undeniable, healthcare organizations often encounter EHR implementation challenges. Let’s discuss the most common barriers to EHR implementation one by one.
Implementation Cost
Financial concerns typically discourage healthcare organizations from EHR integration. However, it is possible to view it as a strategic investment that can yield significant returns. A well-executed integration not only increases efficiency but also leads to profit growth and cost optimization.
Prepare your annual budget in advance for EHR implementation. Despite the initial cost, it can yield future savings by boosting doctor efficiency and enhancing patient satisfaction. According to a Health Affairs study, a typical practice spends approximately $162,000 for EHR implementation, with $85,000 allocated to initial-year maintenance expenses. Although this estimate pertains to the early stages of EHR adoption, it offers a general cost framework. Practices adopting an EHR can typically recoup their investment in about two and a half years.
Data Privacy
Health Sector Cybersecurity Coordination Center states that the healthcare sector encounters a higher frequency of data breaches by cyberterrorists compared to any other industry. Data security breaches can significantly impact not only residents but also senior living establishments and vendors. For instance, in 2022, a lawsuit was filed against a company following a data breach that affected 4.2 million residents across managed care organizations and various healthcare facilities.
When incorporating your EHR, prioritize security measures. Choose cloud-based, HIPAA-compliant platforms to safeguard data and ensure top-level safety.
Usability Challenge
Somе EHR and EMR systеms arе known for their poor functionalitiеs and dеsign. Notifications at inappropriate timеs, issues with еntеring data, and complicatеd navigation prеvеnt thеir practicе application. Thеsе problеms lеad to mistakеs, frustration, and dеcrеasеd productivity. Yеt, this challеngе’s sеriousnеss is typically undеrscorеd by thе potential risks associatеd with compromisеd mеdical data.
For example, David Lareau, CEO of Medicomp Systems, in his Forbes article, suggests involving AI-based technologies. He thinks that AI can improve EHR usability by streamlining workflows and improving access to patient information. Moreover, AI tools can rapidly analyze clinical data from multiple sources. Hence, healthcare professionals can make more informed decisions, improve patient care, and restore smooth workflows.
Lack of Interoperability
Healthcare institutions that lack the EHR work understanding, often incorporate multiple solutions that lack seamless interoperability between them. This creates issues when it comes to sharing patient data across these systems. This complexity can result in errors, redundancies, data duplication, and mismanagement.
To ensure interoperability, choose EHR systems built for it or use middleware for communication between different EHRs. Collaborate with other healthcare providers to establish data-sharing standards. Adopt protocols like HL7 and FHIR, fostering teamwork among EHR systems and vendors to make electronic health record usage seamless and effective.
The Cost of Implementing an EHR System
The cost of implementing an electronic health record system may range from tens to hundreds of thousands of dollars depending on various factors. It depends on the deployment method, EHR implementation strategies, hardware and software choices, the scale of the system, the cost of support, user training, and many others.
Some of those components would be rather pricy, but quite recommended since neglecting them may cost you more in the long run in terms of efficiency or post-deployment costs. To learn more about the cost of implementing an electronic health record system, visit our article on EHR cost breakdown.
How Long Does EHR Implementation Take?
Thе dеvеlopmеnt timе dеpеnds on two things: how largе your hеalthcarе organization is and what you want to accomplish with thе systеm.
For a small dеntal practice that only nееds a fеw things likе booking appointmеnts and uploading documеnts, it could takе about 3–4 months.
But how long does it take to implement an EHR system for a large clinic with many doctors and departments? It could take a year or more. Such a system would have many features, such as sorting by department, linking to calendars and news, and even tools for assessments and communication.
Regardless of how big the project is, you should have a clear plan and timeline.
Сreating a Leadership Team for Successful EHR/EMR Implementation with Empeek
Implementing an electronic health record system in a hospital or any other healthcare institution is a serious decision that will take a lot of time, money, and work to implement. However, it’s all worth the benefits of using this system for both doctors, administrators, and patients. EHR/EMR technology allows clinics and other healthcare institutions to be on the front line of the digital transformation ready to adopt other innovative solutions. That’s why a growing number of healthcare providers are interested in the secrets to successful EHR implementation.
While this article gives you pointers on what to pay attention to at the consideration stage, you need an expert tech vendor to guide you through the whole process with facts and figures that are important and correct to your particular case. This is what we are here for. When you choose the Empeek team for developing and implementing an EHR/EMR solution into your practice, expect a professional, research-based approach at every step. We have years of experience and cases of successful EHR implementation and related medical IT services, and we are dedicated to making a solution that will benefit your practice and set you apart and above the competition. Contact our experts today and let’s talk about the big change for your business.