Remote Patient Monitoring (RPM) is a core component of modern healthcare delivery, with 60.6 million patients using RPM tools in the US in 2024. The adoption of RPM is growing, but so is the complexity of getting reimbursed for offering such services. Healthcare providers must keep up with frequent updates to billing codes, payer requirements, and reimbursement models. Miss a key detail, and you could be losing money, or worse, falling foul of regulations.
This guide covers RPM CPT codes and recent policy updates to help you navigate the remote patient monitoring billing rules.
How Does Remote Patient Monitoring Billing and Reimbursement Work
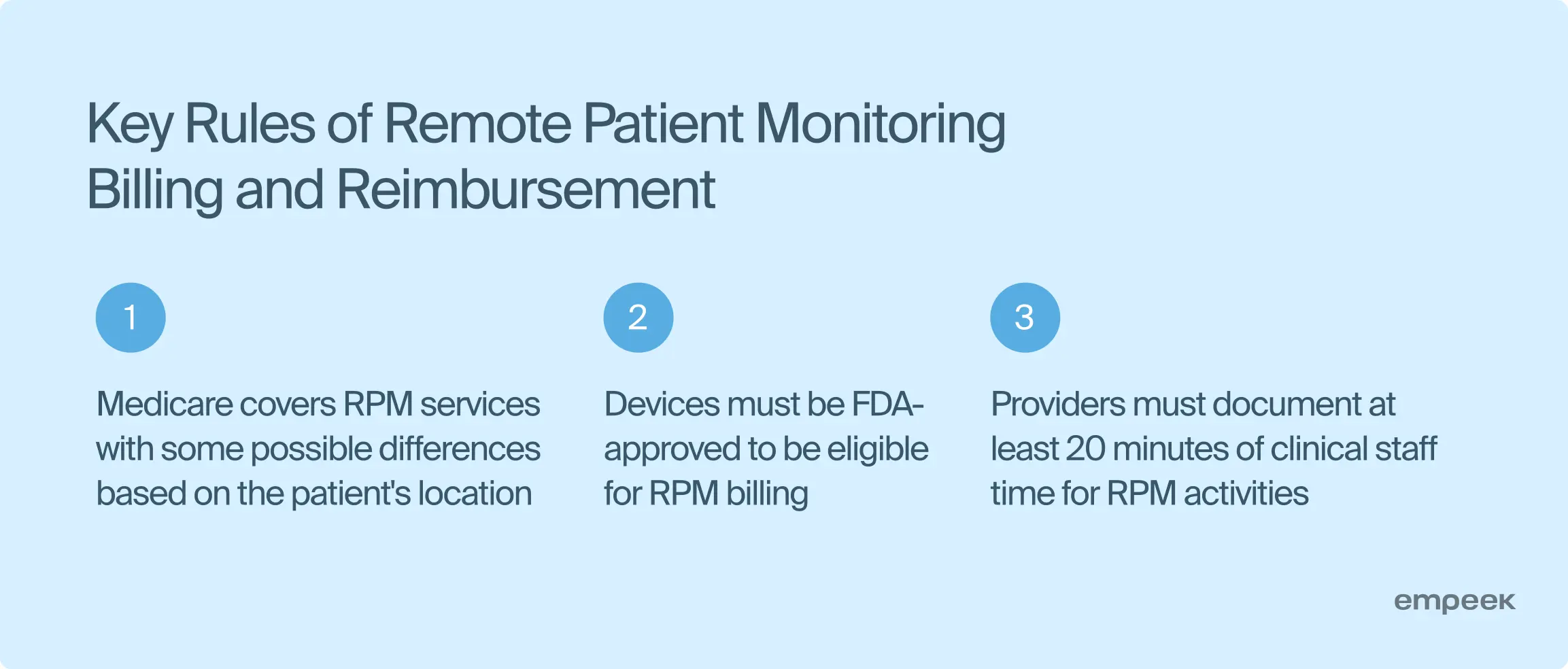
Remote patient monitoring reimbursement appeared to encourage remote healthcare adoption among providers and address the growing need for more effective chronic condition management and post-acute care. Medicare introduced billing codes to compensate providers for remotely monitoring patients, and private insurers soon followed, making RPM more accessible and cost-effective.
RPM in medical billing requires the use of specific Current Procedural Terminology (CPT) codes, which cover services like device setup, data transmission, and patient interaction. Providers document time spent and services delivered to meet payer requirements and receive reimbursement.
To get reimbursed, providers must also use FDA-approved devices and maintain minimum patient interaction, typically 20 minutes per month. Once these criteria are met, providers submit claims, and payers review them based on their policies.
Your next read: How Remote Monitoring Software Disrupts the Healthcare Sector
Recent Changes in Remote Patient Monitoring Billing and Reimbursement
RPM billing rules continue to change as healthcare needs and regulatory guidelines evolve. While 2024 brings only subtle adjustments, updates made during the last few years have significantly impacted RPM billing and reimbursement practices. CMS (Centers for Medicare & Medicaid Services) has clarified several key points regarding RPM (Remote Physiologic Monitoring) and RTM (Remote Therapeutic Monitoring) services in recent regulations:
- 16 Days of Data Collection
Health data must be collected for at least 16 days in a 30-day period for RPM and RTM services. - Established Patients
RPM services are limited to those who have received professional services from the provider within the previous three years (“established patients”). RTM services, however, do not require an established patient relationship. - Billing Limitations
Only one practitioner can bill for specific RPM and RTM CPT codes (99453, 99454, 98976, 98977, 98980, 98981) in a 30-day period.
While 2024 hasn’t introduced drastic changes, you must be aware of the recent updates to stay compliant, keep accurate documentation, and use the medical codes correctly for maximum benefits.
What RPM Services are Reimbursed
RPM services are increasingly recognized and reimbursed by Medicare and private insurers as the need for quality remote healthcare services and tech-driven patient care becomes acute.
To qualify for reimbursement, RPM services must meet specific criteria and you must bill them using the correct remote patient monitoring CPT codes. Generally, reimbursed RPM services fall into four main categories: device setup, data collection and transmission, patient interaction, and care management.

| Device Setup and Patient Education | CPT code 99453 covers the initial setup of an RPM device and instructing the patient on how to use it. This code reimburses providers for the time spent setting up the device, onboarding the patient, and explaining how the monitoring will work. It typically covers a one-time fee for setting up and training. |
| Ongoing Data Transmission and Monitoring | The CPT 99454 code reimburses providers for supplying an RPM device and collecting the patient’s physiological data such as blood pressure, blood glucose, or heart rate. |
| Clinical Review and Patient Interaction | Regular review and communication are crucial aspects of RPM services. CPT 99457 code covers at least 20 minutes per month spent reviewing the patient’s data and providing real-time, interactive communication, such as phone calls or video check-ins. For more complex cases requiring additional time, CPT code 99458 allows providers to bill for each additional 20 minutes. |
| Chronic and Acute Condition Management | While initially focused on chronic conditions, RPM services have expanded to cover acute conditions. Providers can now be reimbursed for short-term RPM used in managing conditions like post-surgical recovery or acute respiratory issues. |
Providers who want to operate more cost-efficiently must understand which RPM services are reimbursed and the corresponding CPT codes. It will allow them to manage reporting and documentation properly to get reimbursement for RPM implementation and support.
Remote Patient Monitoring CPT Codes and How to Apply Them in Your Practice
If you are new to remote patient monitoring, CPT codes are the basics to start with. These are medical nomenclatures used across the US to report healthcare services provided under private and public insurance programs.
Here are the key remote patient monitoring codes with details on what each covers, who qualifies, and how to apply them effectively in your practice.
CPT Code 99453
CPT code 99453 is used for the initial setup and patient education on how to use the RPM device. This RPM code covers the time spent onboarding the patient, setting up the technology, and instructing the patient on using the device for continuous monitoring.
Who qualifies for the CPT code: Any patient who requires ongoing monitoring of chronic or acute conditions qualifies for this code. This includes patients newly introduced to RPM devices for tracking physiological data like blood pressure, glucose levels, or heart rate.
CPT Code 99454
CPT code 99454 is used for the ongoing monthly patient data monitoring and covers the device supply, daily data collection, and transmission to the healthcare provider. This RPM code is billed once per month per patient and covers the operational costs of maintaining the RPM program.
Who qualifies for the CPT code: Patients actively using RPM devices for chronic or acute condition management and whose data is being consistently transmitted qualify for this code.
CPT Code 99457
CPT code 99457 covers up to 20 minutes per month of interactive communication between the patient and the provider. This time includes reviewing the data, making care plan adjustments, and engaging in real-time discussions with the patient about their health metrics.
Who qualifies for the CPT code: Patients who require regular monitoring and intervention qualify for this code. The code applies when the provider spends at least 20 minutes per month actively managing the patient’s care through direct interaction.
CPT Code 99458
CPT code 99458 is an add-on code you can use for each additional 20 minutes of interactive RPM services beyond the initial 20 minutes CPT 99457 covers. This allows for more complex cases where additional patient management time is needed.
Who qualifies for the CPT code: Patients requiring extended time for data review and care plan adjustments qualify. This is particularly relevant for patients with complex health conditions requiring frequent monitoring and communication.
CPT Code 99091
CPT code 99091 is an older code physicians use while collecting and interpreting patient data. It requires a minimum of 30 minutes spent and focuses more on physician-driven analysis rather than ongoing interaction or automated device management.
Who qualifies for the CPT code: This code is typically used for patients requiring a more detailed review and interpretation of transmitted data, often in more specialized care settings.
| Code | Uses and Terms | Amount Reimbursed |
| 99453 | Device setup, patient education, and onboarding | $19.65* |
| 99454 | Monthly device supply, data collection, and transmission | $46.83* |
| 99457 | 20 minutes of patient interaction and care management | $48.14* |
| 99458 | Additional 20 minutes of patient interaction and management | $38.64* |
| 99091 | 30 minutes of data collection and interpretation | $52.71* |
*Amount reimbursed may vary depending on the area
Applying these remote patient monitoring CPT codes accurately in your practice can ensure your services are properly reimbursed while maintaining compliance with payer guidelines. Knowing when and how to use each RPM code is key to running a successful RPM program.
Your next read: Top 10 Benefits of Remote Patient Monitoring and Telehealth in Healthcare
Common RPM Billing Pitfalls
RPM considerably benefits patients and providers, but navigating the billing process can be tricky. Below are four common RPM billing pitfalls that practices should be aware of to avoid claim denials, compliance issues, and lost revenue.
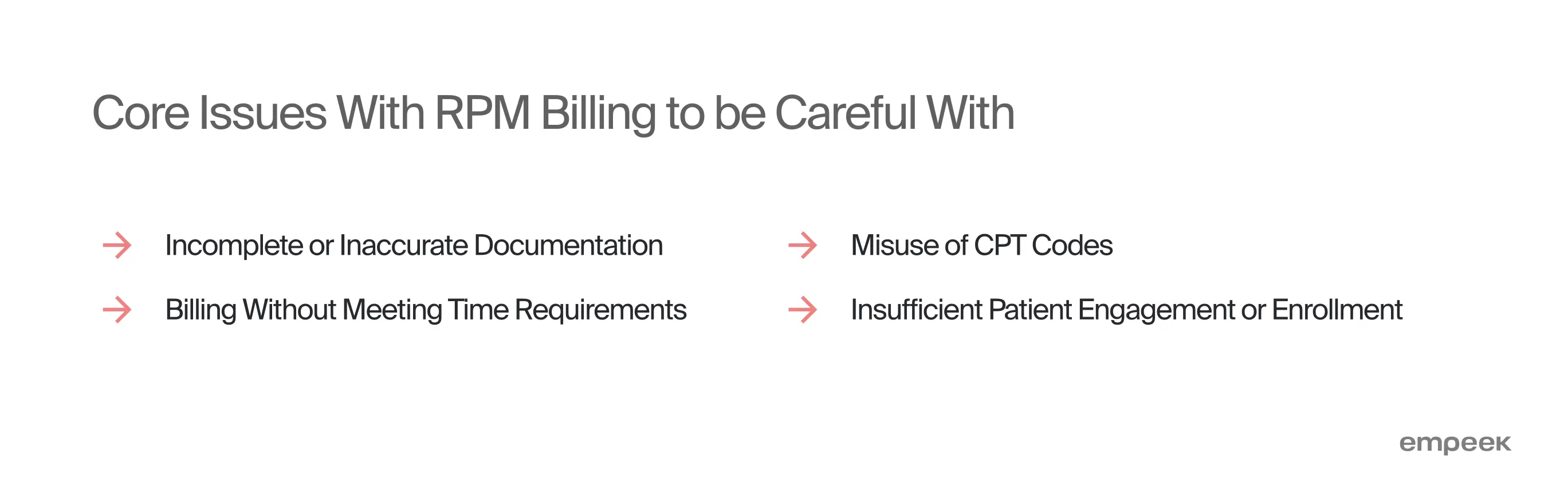
Incomplete or Inaccurate Documentation
One of the most frequent reasons for denied claims is inadequate or inaccurate documentation. For RPM services to be reimbursed, providers must thoroughly document each interaction, the time spent, and the specific services provided. Missing details, such as neglecting to record the time spent on patient interaction or failing to show continuous data monitoring, can result in claim denials. Ensuring detailed, compliant records is key to successful billing.
Misuse of CPT Codes
Another challenge is applying the wrong CPT codes or misunderstanding what each code covers. For instance, billing CPT code 99457 for patient data review without engaging in live communication with the patient is a common error. Each code has distinct requirements and limitations, and providers must understand when and how to use them. Consistent training and staying updated on coding guidelines can help avoid this issue.
Billing Without Meeting Time Requirements
Several RPM codes, such as 99457 and 99458, have specific time requirements providers must meet to qualify for reimbursement. For example, to bill for 99457, at least 20 minutes of patient management, including interactive communication, is required. Billing these codes without meeting the time threshold can lead to audits, recoupment of payments, and potential penalties. Therefore, practices must monitor and track time spent to ensure compliance.
Insufficient Patient Engagement or Enrollment
A less obvious pitfall is failing to engage patients consistently or enrolling ineligible patients. RPM services are designed for continuous monitoring, and if patients do not transmit data regularly or do not meet specific requirements (e.g., not having a chronic condition), billing can be challenged. You must focus on onboarding suitable patients and ongoing support to keep people engaged and adhere to monitoring protocols.
Avoiding these common pitfalls requires careful attention to detail, proper training, and a clear understanding of RPM billing requirements. By proactively addressing these challenges, practices can optimize their RPM programs and secure consistent, compliant reimbursement.
Top Features a Medical Software Must Have to Make Billing Smooth
RPM healthcare software is not just about tracking patient health data; it must also ensure accurate billing and compliance with complex reimbursement requirements. Below are four key features that healthcare software must have to handle the nuances of RPM billing effectively.
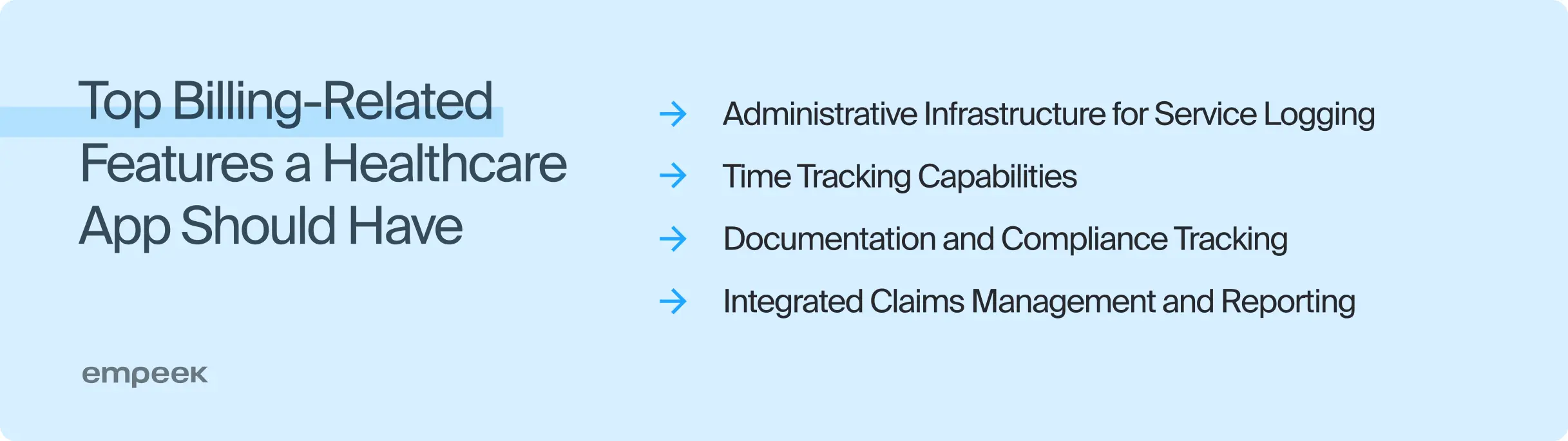
Comprehensive Administrative Infrastructure for Service Logging
To ensure accurate billing, healthcare software must include an administrative backend that logs all RPM services provided. This infrastructure should capture details such as device setup, data transmission, and patient-provider interactions. The software must assign the correct CPT codes to these services and automatically update records as new services are delivered. This functionality helps avoid errors, ensures proper invoicing, and simplifies claim submissions.
Built-In Time Tracking Capabilities
Time tracking is a critical component of RPM billing, especially for codes like 99457 and 99458, which require providers to track the exact minutes spent interacting with patients. Healthcare software must have time-tracking tools that automatically record and log the time spent on patient management tasks. These tools must be able to differentiate between direct patient interactions and other activities like data review to ensure all time requirements are met before submitting claims.
Automated Documentation and Compliance Tracking
CMS remote patient monitoring billing requires strict adherence to documentation guidelines, from recording patient data interactions to ensuring devices meet regulatory standards. Healthcare software must include automated documentation tools that guide providers through compliant data entry to ensure all required fields are completed. Additionally, the software should track whether billing criteria are met, such as sufficient patient interaction and device usage.
Integrated Claims Management and Reporting Features
To streamline the reimbursement process, healthcare software should include integrated claims management features that automatically generate billing reports and invoices based on logged services and time tracked. These features must support direct submission to payers and real-time claim status updates. Additionally, the software must provide detailed analytics and reporting tools to monitor reimbursement trends and identify potential billing issues.
Incorporating these features into healthcare software guarantees correct RPM billing and improves revenue management’s overall efficiency and accuracy. As RPM continues to grow, having software that can manage the intricate details of billing and compliance is crucial for any healthcare provider.
Empeek for Medical Billing Software Development
The Empeek team develops custom medical billing software for remote patient monitoring services. We design systems that automate coding for RPM-related services, claims submissions, and real-time analytics to reduce errors and minimize payment denials.
We can develop a billing solution from scratch or help you integrate an RPM platform with your current systems. Whether you need to connect RPM data with EHR/EMR systems, synchronize patient interactions for accurate time tracking, or link with third-party tools, our integration services ensure smooth data flow and interoperability.
Conclusion
Remote patient monitoring reimbursement programs allow providers to optimize ongoing expenses and make their practices more cost-efficient. So don’t lose your chance to get money back for the quality RPM services you provide. Find a reliable software provider that will help you build or integrate a billing system that optimizes document management, time tracking, and reporting for smooth remote patient care billing and reimbursement.
Contact Empeek to learn more about our healthcare billing engineering services and get a quote for your project.








