Telehealth due to the global pandemic has become more widespread. Internet connectivity and communication in formats like messaging, audio, and video calls can satisfy patients with different illnesses. Stable Internet connections in remote rural areas and other regions should provide excellent healthcare services.
Overview
The development of telecommunication technologies in the 21st century resulted in better healthcare services for everyone. I guess you saw two concepts dealing with telecommunication in the healthcare industry that appeared on the Internet: “Telehealth” and “Telemedicine.” To reduce any confusion about Telehealth and Telemedicine, let’s figure out the difference between them.
Telehealth is a broader term that includes not only Telemedicine but also interactions between medical personnel, supply chain management, and others not related to patient treatment activities using telecommunication technologies.
Telemedicine refers to virtual communication between doctors and patients remotely without visiting medical facilities and using different telecommunication hardware tools (telephone, smartphone, tablet, PC, laptop, etc.) and software (online SaaS, in-house medical software, third-party provider’s software, etc.).
Telemedicine comprises e-health, mhealth, remote patient monitoring using IoT, medical devices, calls with doctors, and online meetings.
Telehealth started in the 1960s in the US. Its primary goal was to create reliable connections between patients in remote rural areas of the country and healthcare professionals. This communication reduces patient transportation costs and allows doctors to make timely healthcare decisions.
For convenience, we can interchange the terms “Telehealth” and “Telemedicine” in this specific paper. Therefore both will mean distant communication using telecommunication tools between medical providers and patients only.
The stigma influenced telehealth development that healthcare services can be efficiently delivered only by physical contact between doctors and patients. But from 2020, when the COVID-19 pandemic started, virtual communication has become a new reality. Healthcare organizations, doctors, and patients conformed to the worldwide healthcare crisis.
Telehealth regulations in different countries were softened due to the coronavirus pandemic. But widespread usage of those tools exposed patients’ healthcare information (PHI) to third parties. So privacy and data protection have become significant issues in Telemedicine. HIPAA, GDPR, PIPEDA, and other regulations require patients’ data protection to reduce the leakage of their healthcare information to other parties due to unauthorized access.
How data leakages affect Telehealth
Information derived from recent reports shows us that violations regarding data access in the healthcare industry occur regularly.
Moreover, they increase every year and threaten the management of medical facilities. Statistics state, “81% of Telehealth Providers Are Concerned About Data Leakage.”
The healthcare industry is much more exposed to hijacking than other economic sectors.
An analysis of data breaches recorded on the Privacy Rights Clearinghouse database between 2015 and 2019 showed that 76.59% of all recorded data breaches were in the healthcare sector. This implies the healthcare sector recorded three times as many data breaches as the education, finance, retail, and government sectors combined.
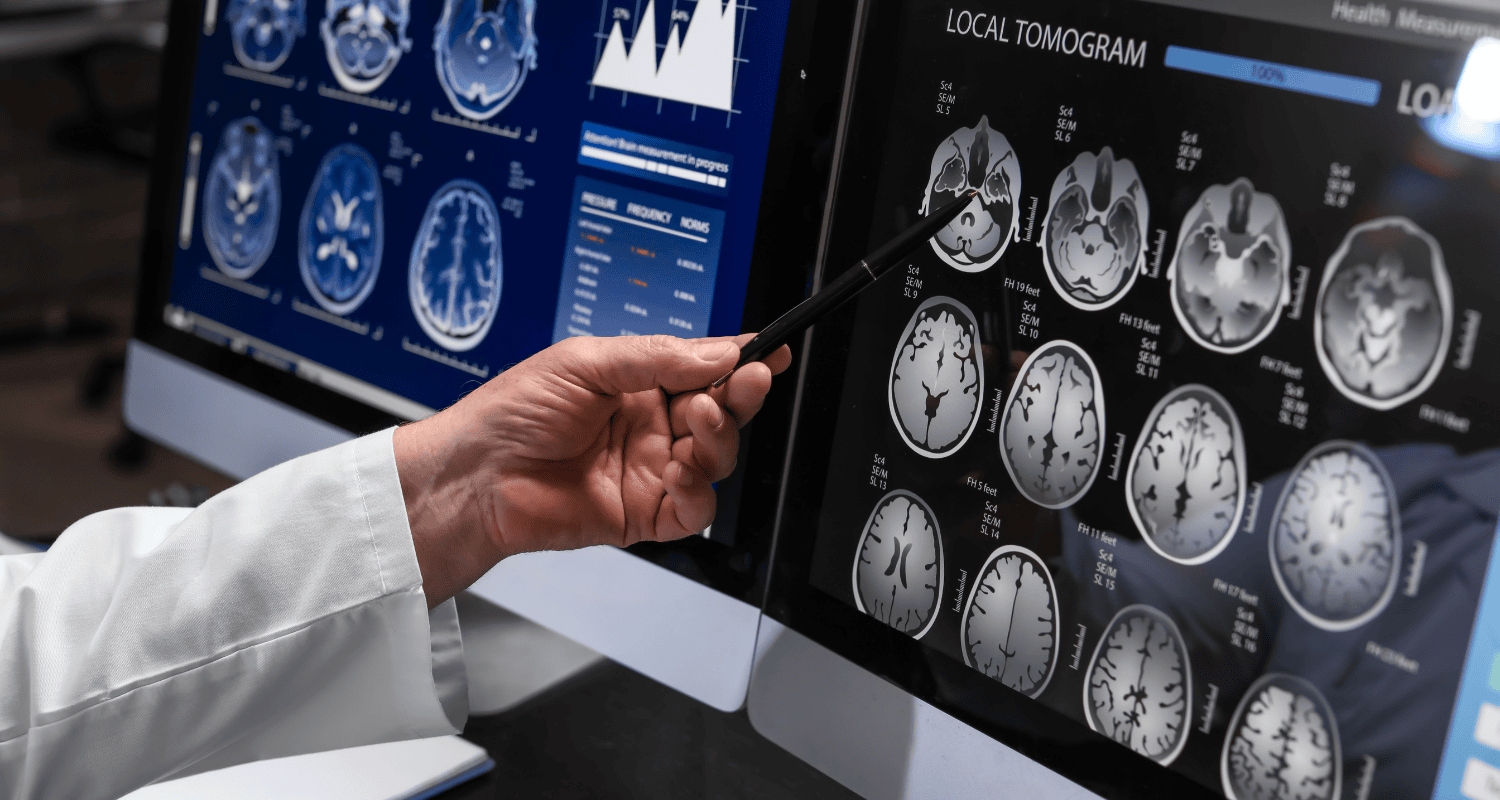
According to Statistica.com, hacking/IT incidents have the most considerable weight among other reasons in all healthcare industries. Check out Figure 1 below.
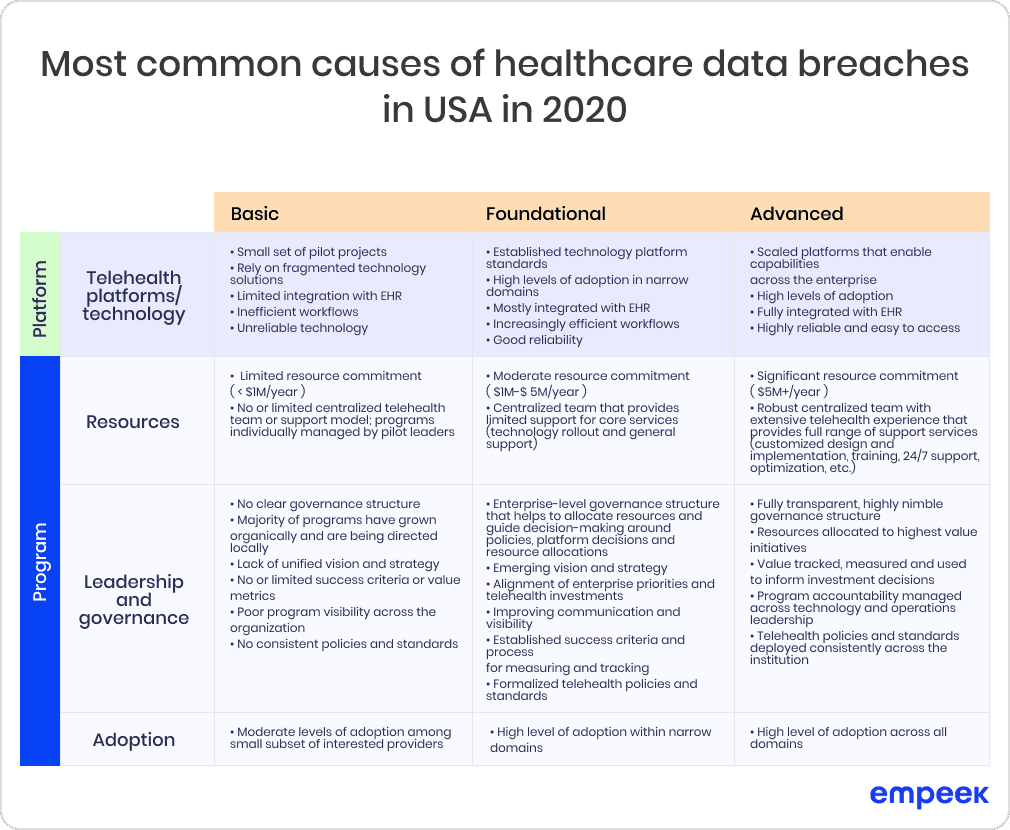
Fig.1: Most common causes of healthcare data breaches in the US in 2020
As we can see on the chart, theft, improper disposal, the loss took less than 12% and hacking/IT incidents, unauthorized access/disclosure are less than 90%. This situation means that cybersecurity plays the leading role in Telemedicine, and its position increases yearly.
Healthcare providers should do some homework to prevent unintended consequences. Recent studies reveal specific steps to lower the number of threats:
“Researchers recommended that healthcare organizations focus on endpoint security, regularly update software, and invest in cybersecurity education to mitigate risk.”
Barriers to Telemedicine adoption
Despite increasing interest in Telemedicine, there are some hindering issues that healthcare providers need to consider. Haleem, A., Javaid, M., Singh, R. P., & Suman, R., Telehealth Equity Coalition, and American Hospital Association reveal the main barriers to Telemedicine implementation:
- Patient privacy. As we mentioned, patients’ data can be exposed to hacking attacks and IT incidents.
- Data accuracy. Healthcare providers are not sure about the correctness of data entered by patients. Senior people, the most vulnerable from the health perspective can’t boast of good digital literacy.
- Cases of misdiagnosis. Patients are worrying if diagnoses made online are accurate.
- Medication intaking control. Sophisticated IoMT devices are needed to track if the patient takes prescribed drugs.
- Fraud and abuse. Patients’ have reasonable fears about untrustworthy relationships with healthcare providers.
- Medical liability. This concept refers to the medical provider’s responsibility for damages to a patient’s health. Medical liability derives from previous items. Any errors done by healthcare facilities regarding misdiagnosis, drug prescription, and fraud can cause detrimental consequences to patients.
- Broadband connection. In rural areas, Internet connection may be unstable.
- Finances. All Telemedicine initial investments may be costly. There are certain restrictions on how Medicare and other payers cover and pay for Telehealth.
- Regulations. Licensure and rules that limit the ability to provide telehealth services.
- Leadership. Lack of leadership and organizational commitment to develop an overarching strategy and integrate it into care delivery.
- Management. Decentralized departmental solutions and pilot programs without governance structure and dedicated leadership.
- Engagement. Inadequate clinical attention and readiness without consideration of human factors in the user experience and workflows for both clinicians and patients.
- KPIs. Evolving measures of success and critical performance indicators hamper scaled platforms.
- Old habits. Aged people are accustomed to communicating with doctors face to face, so transitioning to newer technological innovations is a complex psychological process.
Business models for Telemedicine adoption
There are specific business models for Telemedicine adoption. One of them is the so-called “provider-to-provider” model. This notion is based on the idea that healthcare providers can share their resources, knowledge, and experience. Therefore they reduce or eliminate workforce deficit efficiently using healthcare professionals’ potential. This model can be effective for different medical boards, conferences, and meetings to share medical expertise between medical specialists.
Successful implementation of the “provider-to-provider” model depends on the medical facility’s management’s willingness to provide high-end patient care.
As Pereira F., one of the Telemedicine experts, says:
“One of the most significant challenges related to the adoption of telehealth is not technology-based but “people-based” issues and involves its integration with current workflows.”
Another existing constraint for such a Telehealth model establishment is connected to finances. As researchers proclaim:
“While the majority of new research examined outcomes related to patient and provider experience, the population health and cost measures continue to be limited and require further development.”
Remote patient monitoring, mHealth, and virtual care for patients comprise a direct-to-consumer model. Physicians communicate with patients via the Internet platforms directly. They use mobile phones, tablets, PCs, laptops, and any devices for outlying communication aid patients in receiving timely treatment. Synchronous and asynchronous methods include videoconferencing, audio calls, store-and-forward, emails, chats, and other means of telecommunication. There are many use cases for such a model in healthcare: pharmacy, chronic care management, Tele-ICU tools, specialty medicine consultations, and others.
There are several limitations even to this method. As C. Kimble says that e-health raises particular challenges for the evaluation of business models: Systems may have multiple uses, and joint costs are difficult to apportion; the existence of a system in one part of an organization may lead to expanded use in another; and, as with most ventures connected to IT, technological change can rapidly make existing ideas outdated.
The Complex Approach for Telehealth
Telehealth is an ongoing concept, which will be constantly actual since telecommunication technologies exist. So a systematic approach should be used here. One of the most relevant complex and systematic methods is VISOR. This approach stands for
1) Value, which the provider gives to customers;
2) Interface, which connects consumers in a user-friendly manner;
3) Service platforms, which sustain the robust connection between doctors and patients;
4) Organizing model to optimize processes and relationships;
5) Revenue/cost model, which is suitable for every partner.
This model is illustrated below (see Figure 2):
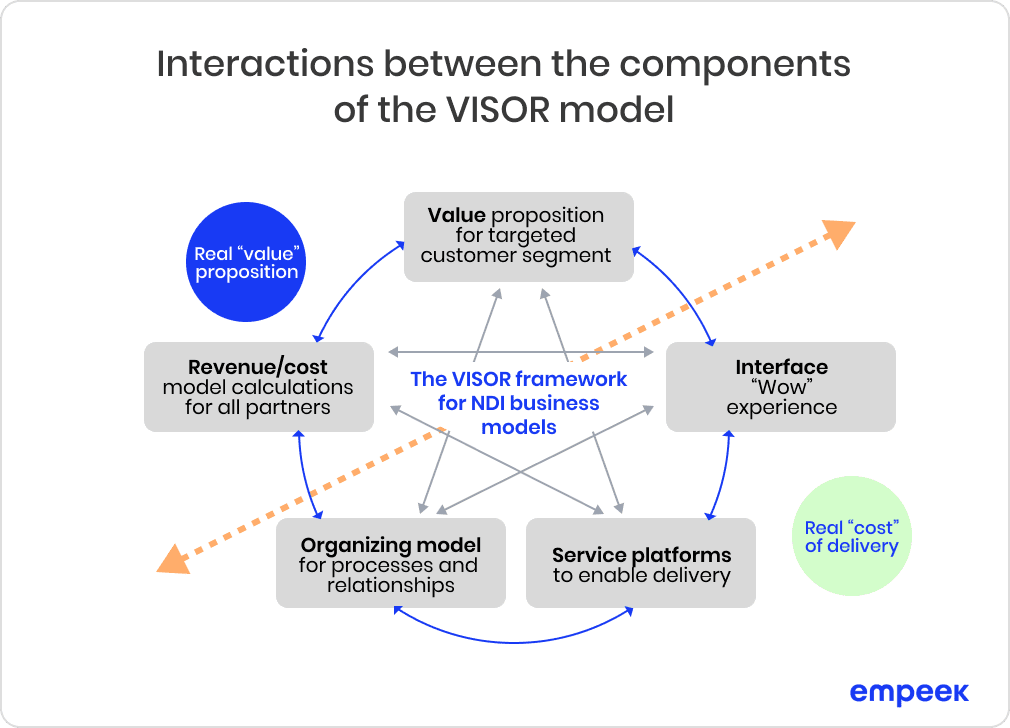
Fig. 2: Interactions between the components of the VISOR Model.
Abbreviation: NDI, Networked Digital Industry.
The “provider-to-provider ” and “direct-to-consumer” models are used only in their specific domains. While the VISOR model is universal and refers to each depending on the value, it brings to the customer. The latter model considers the interests of every party: customers, healthcare providers, doctors, technicians, and others. The first two models may omit the interests of specific partners. Any clinic may utilize the VISOR model since it allows them to plan and distribute limited resources and provide value-based patient care.
Hospital Maturity Telehealth Model
According to research by the AHA Center for Telehealth, the innovation level of Telehealth adoption can be “Basic,” “Foundational,” and “Advanced.” The main components for a proper Telehealth establishment are “Telehealth technologies and platforms,” “Resources,” “Leadership and governance,” and “Adoption” (see Figure 3).
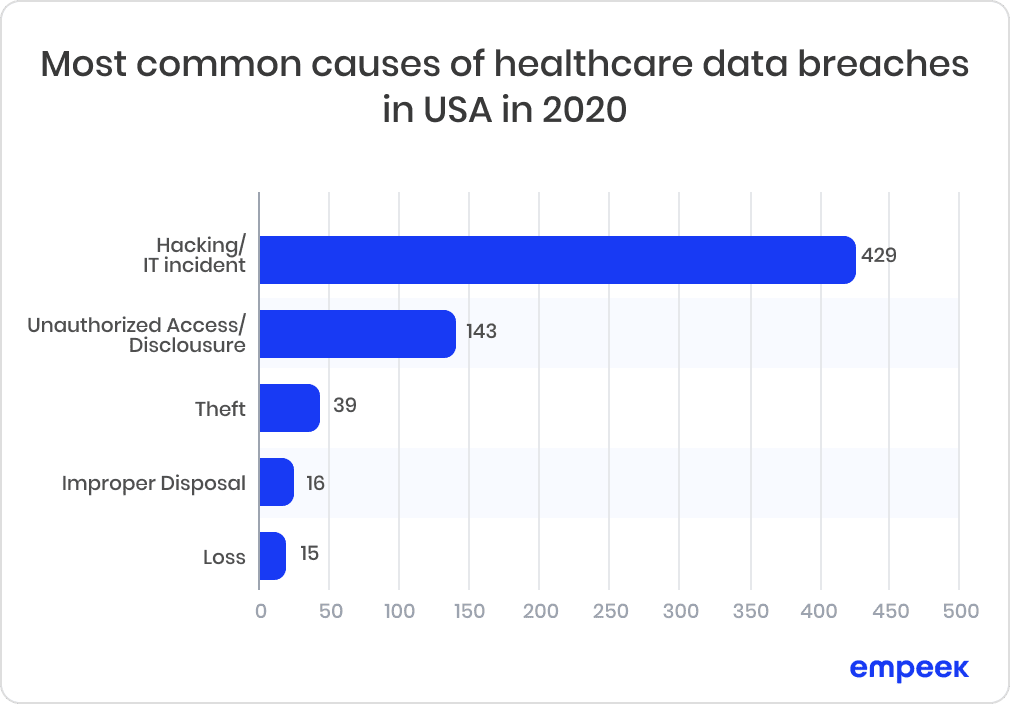
Fig. 3: Hospital Maturity Telehealth Model
Francis Pereira, a Telehealth expert, says that “rapid telehealth adoption can only be achieved when, on the one hand, the service platform, (perhaps more importantly) the organizational and revenue model, and on the other the interface and to a lesser extent value proposition are all adequately addressed.”
How the VISOR model benefits Telehealth
Starting in 2020, with the COVID-19 pandemic, many regulators, e.g., in the US, allowed providing more than 140 medical services via Telehealth. After such moves, new fraudulent schemes emerged. Most of them refer to Telehealth individuals involved in scams. They receive kickbacks and bribes for prescribing unnecessary drugs or durable medical equipment (DME) without specialist consultations, mainly for seniors who participate in Medicaid and Medicaid.
The whopping figures depict severe issues with healthcare data breaches compared with other industries. Figure 7 shows more than 7.13 mln USD average cost of data breaches worldwide in 2020.
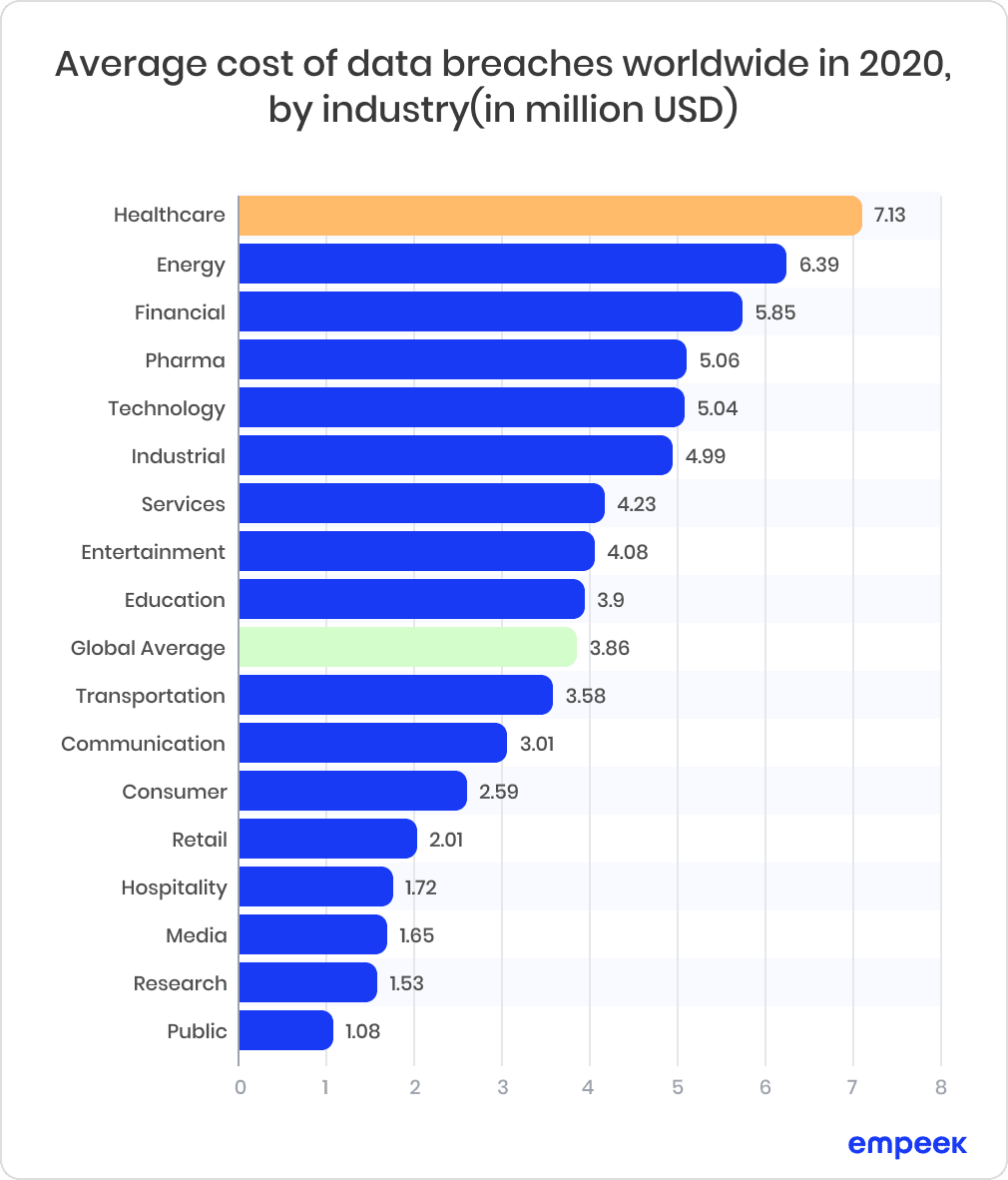
Fig. 4: Average Cost of Data Breaches Worldwide in 2020, by Industry (in million USD)
Patient-oriented models enable customers to control the quality of provided services. According to the VISOR scheme, patients can choose healthcare providers and doctors based on feedback, reviews, and other information. Most medical facilities are interested in fair, supportive aid and reliable communication with their patients.
Support teams can help customers to avoid fraudulent schemes and scams. Governmental organizations and clinics can recommend how to analyze information and report suspicious people or entities.
According to Scamcatchers.com, there isn’t too much that Medicare beneficiaries can do to protect themselves from the rise of these scams:
“These scammers are taking advantage of the medical equipment field and Medicare, not necessarily the patients themselves.”
But Ben Bush states in the article:
“If you feel that you received a call from someone posing as a telemedicine representative or consultant, contact a lawyer immediately. The more beneficiaries that report fraudulent behavior, the quicker these scams can be thwarted.”
Even if you don’t encounter scams in Telemedicine, you may be endangered by pharmacy. Customers, because of misdiagnosis, can receive medical prescriptions that can harm patients and lead to disease readmission and health deterioration.
Physicians tend to suggest patients visit medical facilities to avoid misdiagnosis risks. Nurses or other medical specialists can help doctors when contacting an ill person online. Such methods don’t work in times of severe pandemic or when clinics don’t have many human resources.
The VISOR scheme enables medical specialists and patients’ education about possible threats in Telehealth and how to limit them, accurately diagnose during video calls for specific medical specialties, etc. So this model enhances the quality of medical services by providing necessary tools for doctors and patients.
Doctors’ education is an obligatory part of their work. Right now, it refers to online communication with patients. As Judy George says:
“Many medical societies have begun offering education about remote exam techniques specific to their specialties.”
Cybersecurity remains the #1 concern among healthcare providers. According to IBM, the cost of a typical healthcare breach rose to an average of $9.4 million in 2021, an increase of $2 million over the previous year. The average ransomware attack on healthcare costs $4.6 million per incident.
According to SafetyDetectives, most U.S. healthcare organizations allocate a tiny fraction of their IT budget to cybersecurity. In 2020, healthcare cybersecurity professionals were asked how much of their IT budget was spent on cybersecurity. Many didn’t even know. The chart below shows minuscule spending by the US healthcare providers on IT security (see Figure 5).
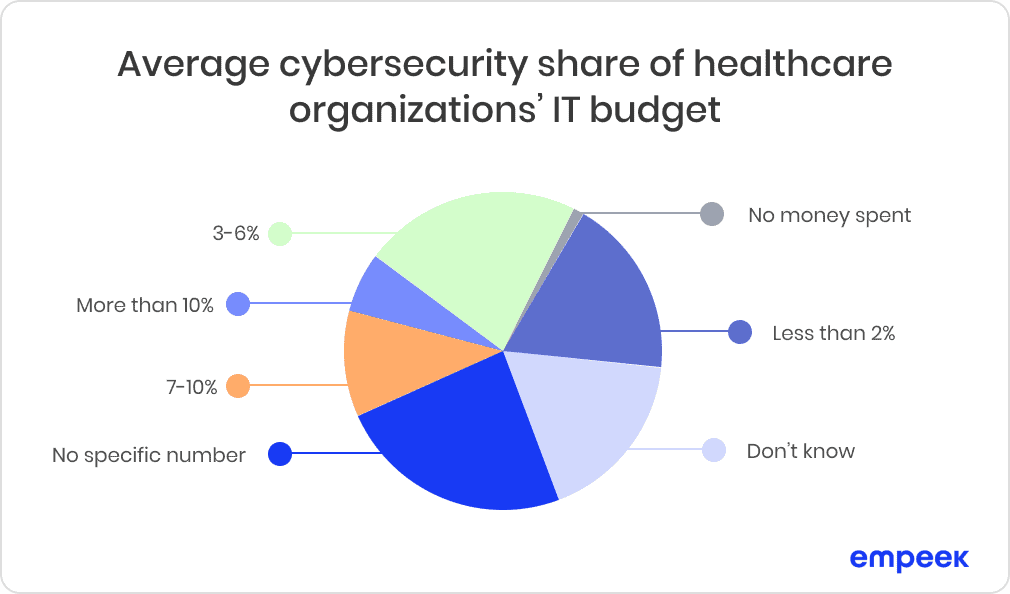
Fig. 5: Average cybersecurity share of healthcare organizations’ IT budget
Service platforms must be a reliable gateway for customers. Patients’ data should be secured by two-factor authentication, strong logins, and paroles. According to the VISOR scheme, the IT partner organizes firewalls, separate networks, and other means of data and privacy protection as a “cost” part of the equation.
The healthcare institution provides Telehealth services as this model’s “value” component. They should also educate and consult patients, especially seniors, on protecting their medical data from possible phishing, malware, and other cybersecurity threats.
Hospital & Healthcare Management magazine says, “It is important for medical practices to take a comprehensive approach to cybersecurity with solutions — during the COVID-19 pandemic and thereafter.”
Innovative Telepsychiatry model
Telehealth market is flooded by dozens of platforms that provide remote patient monitoring, mHealth, and media between patients and clinics. But the creative approach to effective communication within patients’ communities is uncommon to users.
There is one platform, which is called Mood Lifters. It aids patients with mental health issues in controlling their physical state and uplifting their moods. According to NAMI, the National Alliance on Mental Illness, based in the US, 21% of U.S. adults experienced mental illness in 2020 (52.9 million people). This proportion represents 1 in 5 adults. 5.6% of U.S. adults experienced severe mental illness in 2020 (14.2 million people). This share represents 1 in 20 adults.
The company hired world-class scientific advisors as mentors for mental health disease programs within this platform. They teach students practical strategies they can implement in their lives and share with newcomers to Mood Lifter’s community. Members of a particular group share their experiences. Leaders of this community among patients themselves guide other group members. So they start to believe that they can overcome their specific illness.
How community members resolve mental issues through Telehealth
The Mood lifter’s programs track patients’ improvements or any other changes in their behavior due to the check-in process. They need to fill in a questionnaire so mentors know if patients succeed with their tasks.
Weekly online meetings help users with sleep strategies, the importance of exercise, improving relationships, controlling your emotions, changing your negative thoughts, and increasing joy and contentment.
Creators of this program use gamification to encourage its members to progress with their mental well-being. Participants gain points for taking part in activities assigned in meetings. The goal is to implement successful behavioral strategies into digestible everyday habits.
In the end, detailed patient progress analysis and effective motivation techniques significantly improve their mental health.
All methods mentioned above for mental health treatment create a productive and friendly patient environment. Another benefit of Mood Lifter’s program is peer support. Graduates of previous mental health healing programs help new participants with their tasks.
New members respect such “coaches.” They see people similar to them. Newcomers start to believe that they can go through and achieve their own goals as their predecessors did.
Such motivation is much more effective than the mentorship of certified specialists. The authoritative person with lots of experience would discourage participants. They would think they need to read dozens of books, watch tons of video content and do a lot of hard work to resolve their issues. So the results for such patients would decrease.
But evidence-based mental health care reduces judgemental stigma and aids patients in doing the opposite – succeed in this program.
The main advantages of the innovative mental healthcare platform are its cost-effectiveness and scalability. You don’t need to hire extra staff to teach, control, and guide program members. Peer leaders do the majority of all necessary work.
Effective organizational structure, treatment process, technology, and resource usage expand the idea of mentally healthy, happy people far beyond one region or company. Many institutions across the US and other countries can use this solution to change the lives of thousands and thousands of people from low-income families, regardless of race, ethnicity, gender, sexual orientation, etc.
Numerous schools, colleges, foundations, universities, and other institutions can be involved in the vital processes of mental health treatment.
Local businesses can be satisfied because their staff members become more attentive at work, productive, and highly motivated. Thus companies’ efficiency, customer service, and income increase.
Several Telehealth experts highlight such effectiveness of value-based models. Innovative and cost-effective telehealth solutions improve quality care and near- and long-term health outcomes for individuals while controlling costs.
Conclusions
Only complex value- and evidence-based solutions, including organizational, service platforms, interface, and rich-value proposition for targeted customer segments, can bring Telehealth to the top-notch level in the nearest future. The VISOR model provides complex and well-structured Telemedicine solutions for medical facilities.
Create your Telehealth system, which will satisfy customers’ needs and the medical organization’s management requirements.